To better assess the efficacy of drugs in early tumor response in clinical trials involving novel cancer therapeutics through PET imaging, researchers from a top U.K. center, Germany, France, and the U.S. have proposed a series of recommendations. Also, their analysis of previous research found early FDG uptake may help in estimating perfusion and tumor vascularity, but they cautioned additional work is needed to confirm the FDG-PET technique's value.
In a paper published online on 5 April in European Radiology, lead author Dr. Eric Aboagye, PhD, director of the CRUK-EPSRC-MRC-NIHR Comprehensive Cancer Imaging Centre and head of the CSC Molecular Therapy group at Imperial College London, noted that dynamic [15O]-water is considered the gold standard method of studying tumor blood flow in patients. While initially the water-PET method directed patients to inhale water-carbon dioxide (CO2), which was converted to water in the lungs, the technique has been replaced by a dynamic PET protocol that injects a bolus containing water into a peripheral vein followed by a dynamic PET scan of the target tissues for as long as 10 minutes.
Quantification of tissue blood flow is measured by imaging a major blood vessel, such as the order of the left ventricle, or in peripheral arterial blood samples.
Several previous studies have also used water-PET to monitor the delivery of radiolabeled drugs to target the tumor. The radiolabeled drug, in turn, provides data or pharmacokinetics, whereas the water-PET gathers information on whether the agent in combination of treatments has different effects on tumor perfusion.
New radiotracers that target integrin receptors expressed on the blood vessels including fluciclatide-18F and galacto-RGD-18F are promising agents for imaging vascularity.
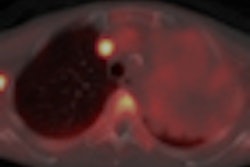
In a comparison of FDG-PET and water-PET, one study found that imaging blood flow two minutes after FDG injection was highly comparable to results with water-PET, suggesting FDG may provide a satisfactory estimate of perfusion in tumors, the authors wrote.
FDG-PET imaging may also help predict decreases in blood flow. Citing three breast cancer studies, Aboagye and colleagues wrote FDG uptake and changes in blood flow were associated with response to chemotherapy. "Indeed, three studies have indicated that FDG-PET may be useful for assessing experimental agents that affect tumor vascularity," they stated.
The researchers also recommend exploring more quantitative approaches, such as dynamic imaging, to study tumor vascularity. The validity of standard uptake values (SUV) as a measurement variable should be confirmed for new radiotracers before use, they wrote. To better validate results from such research, a group of European and North American researchers and the Experimental Cancer Medicines Center Imaging Group developed guidelines to better direct clinical trials.
The researchers also advocated adopting regular testing procedures and periodically logging in data from scanners to a common archive for testing and verifying analysis procedures.
For the benefit of patients, they recommended monitoring radiation dose for a particular trial. "This should be realistic, but not too restrictive," the authors wrote. "The risk to the study group in question should be evaluated by a qualified medical physics expert."
Also, consider different radiotracers, which could target physiology and measure tumor vascularity, as well as agents, such as FDG that indirectly may detect changes in tumor vascularity, they urged.
As more information becomes available, Aboagye and colleagues suggest developing a comprehensive imaging database for the imaging community as a whole and to start sharing PET phantom data to test and validate the database. They also recommend using technology resources from the U.S. National Cancer Institute to expand the database.
Misregistration and motion also are frequent problems specific to PET/CT that can "contribute significantly to error and/or image blurring," the authors noted. Since it is standard practice to evaluate nonattenuation-corrected PET images for artifacts, they recommend researchers average cine CT for attenuation correction of respiratory average PET data, with careful attention paid to radiation dose. Researchers should consider using tumors larger than 2 cm in size to reduce partial volume effects, since lesions smaller than 2 cm can adversely bias results, based upon imaging resolution.