Dutch researchers have used positron emission tomography (PET) to predict how much of an anticancer drug is absorbed by a tumor. In a preliminary study in lung cancer patients reported today in Dublin, they revealed that less than 1% of the drug docetaxel is absorbed by the tumors.
"This finding underscores the fact that only a small amount of drug accumulates in tumors and indicates that there is an urgent need for strategies that selectively enhance drug delivery to tumors. For that purpose, the direct effects of other, anticancer drugs on metabolism as well as drug delivery to tumors need to be investigated, as other drugs may also affect metabolism and drug delivery to tumors," Dr. Astrid van der Veldt, PhD, from the VU University Medical Center in Amsterdam, told attendees at the symposium organized by the European Organization for Research and Treatment of Cancer (EORTC), National Cancer Institute (NCI), and the American Association for Cancer Research (AACR).
The group used PET to track very small tracer doses of docetaxel, which had been radiolabeled with the positron emitting radionuclide carbon-11, in the patient. The PET scan was able to follow this C-11 docetaxel dose in the body noninvasively and provide information on how much reached the tumor, the amount absorbed by the tumor, and its effect on the tumor. By using a microdose of docetaxel in this way, the patients were protected from any drug-induced toxic side-effects that could occur if the docetaxel was administered at therapeutic doses.
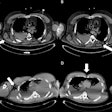
Amount of docetaxel uptake in tumors
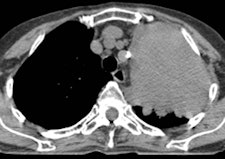
![An example of a patient with non-small cell lung cancer showing relatively high C-11 docetaxel uptake in a tumor with a volume of 334 cm3. During the therapeutic scan, the patient was treated with 110 mg of docetaxel. Left: CT scan showing tumor. Right: PET/CT fusion image of a therapeutic C-11 docetaxel summed image [25-65 min; mean C-11 docetaxel Ki = 0.0125 mL·cm-3·min-1; total accumulated amount of cold docetaxel at 90 min = 543 µg (at 1.62 µg·cm-3), corresponding with 0.49% of the infused dose docetaxel]. Images courtesy of Dr. Astrid van der Veldt, PhD.](https://img.auntminnieeurope.com/files/base/smg/all/image/2012/11/ame.2012_11_08_11_54_06_622_2012_11_08_PET_CT_pic2.png?auto=format%2Ccompress&fit=max&q=70&w=400) An example of a patient with non-small cell lung cancer showing relatively high C-11 docetaxel uptake in a tumor with a volume of 334 cm3. During the therapeutic scan, the patient was treated with 110 mg of docetaxel. Left: CT scan showing tumor. Right: PET/CT fusion image of a therapeutic C-11 docetaxel summed image [25-65 min; mean C-11 docetaxel Ki = 0.0125 mL·cm-3·min-1; total accumulated amount of cold docetaxel at 90 min = 543 µg (at 1.62 µg·cm-3), corresponding with 0.49% of the infused dose docetaxel]. Images courtesy of Dr. Astrid van der Veldt, PhD.
An example of a patient with non-small cell lung cancer showing relatively high C-11 docetaxel uptake in a tumor with a volume of 334 cm3. During the therapeutic scan, the patient was treated with 110 mg of docetaxel. Left: CT scan showing tumor. Right: PET/CT fusion image of a therapeutic C-11 docetaxel summed image [25-65 min; mean C-11 docetaxel Ki = 0.0125 mL·cm-3·min-1; total accumulated amount of cold docetaxel at 90 min = 543 µg (at 1.62 µg·cm-3), corresponding with 0.49% of the infused dose docetaxel]. Images courtesy of Dr. Astrid van der Veldt, PhD.A potential problem was that the behavior of 11-C docetaxel in the tumor at tracer doses may be different from its behavior at therapeutic doses, noted van der Veldt. Therefore, she investigated whether a PET study using tracer doses of C-11 docetaxel could predict tumor uptake of docetaxel at therapeutic doses.
Six lung cancer patients who had not been treated previously with docetaxel underwent two PET scans: one with the tracer dose of docetaxel, and another during a combined infusion of a tracer dose and a therapeutic dose (75 mg/m2) of docetaxel. The researchers compared the tumor uptake of both the tracer and therapeutic doses of docetaxel and found that the tracer dose correctly predicted the tumor uptake of the therapeutic dose.
According to Dr. Stefan Sleijfer, PhD, scientific chair of the EORTC-NCI-AACR symposium: "This study is interesting because it provides more insight into the amount of drug that reaches the place where it should go: the tumor cell. Because of technical limitations, this is a relatively unexplored field of research, which is of great importance. Eventually, this may lead to better prediction of outcome and novel combinations augmenting the penetration of active antitumor agents into the tumors."
The study showed that microdosing data from PET scans of C-11 docetaxel could be used to reliably predict tumor uptake of docetaxel during chemotherapy, which was also associated with tumor response to docetaxel therapy, explained van der Veldt. The findings warrant larger clinical studies investigating the predictive value of initial C-11 docetaxel uptake for tumor response to docetaxel therapy.
In addition, the present study provides a framework for investigating the PET microdosing concept for other radiolabeled anticancer drugs in patients with other cancers, she said. She thinks this study is the first in which absolute tumor uptake of chemotherapy was measured noninvasively in patients.
Additional analyses revealed that less than 1% of the therapeutic dose of docetaxel that was infused in the patients was finally taken up by the tumor tissue. This uptake might also be affected by other drugs that are being delivered at the same time.
"Although, at present, C-11 docetaxel PET cannot be used on a large scale because of its complexity and high costs, it is a promising technique for several investigations," van der Veldt said. "C-11 docetaxel PET may be useful to predict response to docetaxel therapy and select patients for docetaxel-containing treatment strategies, thereby contributing to more personalized treatment planning in individual cancer patients. In addition, C-11 docetaxel PET may help to define the optimal design of large clinical trials to investigate the effects of drug scheduling on efficacy in cancer patients."
The research was funded by the Cancer Center Amsterdam.