The fusion of metabolic and morphological data should improve diagnostic accuracy, but mistakes can still occur. Some malignancies that have a low affinity to FDG may be missed if the corresponding CT scan is not scrutinized carefully, and changes induced by radiation treatment and/or chemotherapy can lead to restaging PET/CT scans being misinterpreted.
Irish researchers have reported that PET/CT imaging using F-18 FDG glucose analogue can be a useful examination to diagnose and stage cancer, but because F-18 FDG is not tumor-specific, its activity may lead to a misdiagnosis.
Malignant tumors have a higher metabolic rate and generally express higher numbers of specific membrane transporter proteins than normal cells. While F-18 FDG is seen in tumor cells, not all tumors take up FDG. And because glucose acts as a basic energy substrate for many tissues, F-18 FDG activity can be seen both physiologically and in benign conditions. This can lead to false-positive and false-negative interpretations.
In their article published online on 9 September in Insights into Imaging, Dr. Niamh Long and Dr. Clare Smith of the department of radiology at Mater Misericordiae University Hospital in Dublin, identify specific postcancer treatment conditions that may lead to false-negative and false-positive findings. By being aware of these conditions, and correlating the PET and CT components, unnecessary biopsies, overstaging, and misdiagnosis may be prevented.
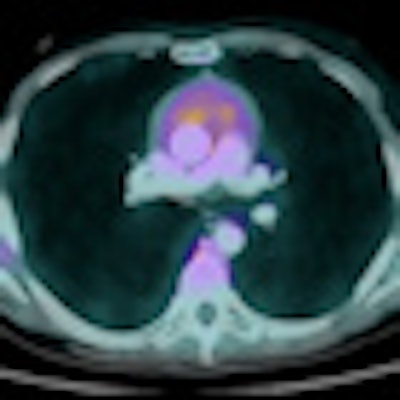
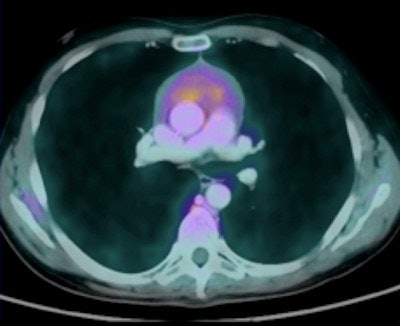 Postchemotherapy imaging of a mediastinal lymphoma. Axial image shows contrast-enhanced chest CT, registered and fused with FDG-PET. Metabolic and structural information can be evaluated in a single image. All images courtesy of Dr. Arturo Chiti, Humanitas Clinical Institute, Milan.
Postchemotherapy imaging of a mediastinal lymphoma. Axial image shows contrast-enhanced chest CT, registered and fused with FDG-PET. Metabolic and structural information can be evaluated in a single image. All images courtesy of Dr. Arturo Chiti, Humanitas Clinical Institute, Milan.Technical causes of false positives
Differences in breathing patterns between CT and PET exam imaging can cause misregistration of pulmonary nodules on fused images, particularly at the lung bases. CT scans of the thorax are generally performed during a breath-hold, while PET images are acquired during tidal breathing. The authors recommend that acquiring CT images of the thorax during quiet respiration will help reduce artifacts.
Injection of a radioactive clot following blood withdrawal into a syringe when radiotracer is being administered can result in pulmonary hotspots. This area of abnormal uptake should be scrutinized in subsequent CT exams.
Subcutaneous tracking of FDG along lymphatic channels in the arm can occur if there is leakage of radiotracer in the subcutaneous tissues at the injection site. Injection artifacts may be identified as a result of this. The authors advocate injection at the side contralateral to the site of the disease, particularly for breast cancer patients, to facilitate differentiation between artifactual and metastatic uptake.
Radiologists should be aware that metal in the body degrades the quality of a CT image and may produce streak artifacts.
Confusing FDG activity with malignancy
Adrenal adenomas, adrenal hyperlasia, and angiomyolipoma are causes for false-positive adrenal lesions. Evaluation of the CT component of the exam may provide additional diagnostic information to prevent this.
Thyroid update occurs in about 4% of exams. Further investigation with ultrasound and tissue biopsy is recommended. Additional testing is also true when endometrial uptake occurs in postmenopausal women. Endometrial uptake of FDG varies cyclically and is increased both at ovulation and during the menstrual phase of the cycle.
Physiological uptake within the gastrointestinal tract is highly variable, especially in the colon. Focal areas that are of greater intensity than background liver uptake may represent a colonic neoplasm, and should be further investigated. Low-grade linear uptake in the gastrointestinal tract is most likely related to smooth muscle activity and swallowed secretions. High uptake in underdistended or overlapping loops of bowel may contribute to misdiagnoses of the small bowel.
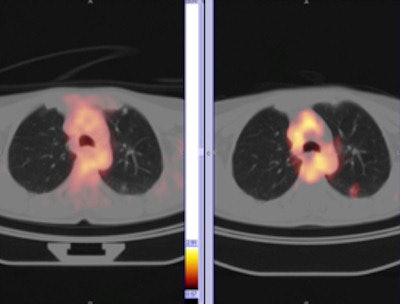 Metabolic characterization of a lung nodule in the left lower lobe. FDG-PET (left panel) shows no uptake, indicating that the glucose metabolism is not elevated in the nodule. Carbon-11-methionine PET reveals increased metabolic activity in the lung lesion. Pathology confirmed the nodule as a bronchoalveolar carcinoma.
Metabolic characterization of a lung nodule in the left lower lobe. FDG-PET (left panel) shows no uptake, indicating that the glucose metabolism is not elevated in the nodule. Carbon-11-methionine PET reveals increased metabolic activity in the lung lesion. Pathology confirmed the nodule as a bronchoalveolar carcinoma.Hypermetabolic brown adipose fat is a common cause of a false-positive diagnosis. It is more prevalent in women and children, and occurs more frequently during cold weather and in thin patients with a low body mass index.
The authors recommend that patients be given blankets and administered the F-18 FDG in a warm room. Oral propranolol also may be administered.
CT images should be separately evaluated to assess lymph nodes when brown fat surrounds them. If the morphology of the lymph node is normal, increased uptake can be attributed to brown fat and malignancy can be confidently excluded. Radiologists should also be aware that atypical brown fat in the mediastinum can be misinterpreted as nodal metastases.
Treatment-related causes of false positives
Pneumonitis induced by radiotherapy can cause increased uptake. Radiologists should know when radiotherapy treatment took place and the radiation doses administered. Increased uptake should be correlated with CT images to avoid making a false-negative diagnosis.
Patients with anal, colorectal, gynecological, and prostate cancers may develop pelvic insufficiency fractures, particularly if they have osteoporosis. These fractures may be difficult to differentiate from bone metastases. However, there are differential features and suspected insufficiency fractures demonstrate a reduction in FDG uptake over time when additional exams are performed.
Patients who've had surgical procedures in addition to radiotherapy treatment may exhibit nontumor related uptake at postoperative wound sites, colostomy sites, or the site of postradiation inflammatory change. To minimize this, the authors recommend that the exam not be performed for at least six weeks following surgery and/or completion of radiotherapy treatment. If uptake still is seen, radiologists need to evaluate CT images in these regions, being aware that uptake of FDG at these sites may also mask malignant uptake in neighboring areas.
Radiologists should also be informed if a patient has had a talc pleurodesis, a procedure for the treatment of persistent pneumothorax or pleural effusion. The inflammatory reaction from the procedure can cause increased FDG uptake.
Patients who've had chemotherapy treatment may be at increased risk of infection due to bone marrow suppression. Infection is a major cause of a false-positive diagnosis. Postchemotherapy thymic hyperplasia may also be seen within 12 months of treatment. Osteonecrosis is a common toxicity following chemotherapy and when visualized in the mandible, from tooth extraction. It also causes FDG uptake.
Bone healing causes flare activity, a disproportionate increase in bone lesion activity. While a rare phenomenon, scans that show this need to be interpreted with caution.
Osteoblastic metastases
Osteoblastic and sclerotic metastases are two types of bone metastases that are commonly not identified in F-18 FDG-PET imaging because they poorly concentrate the FDG. Sclerotic metastases can be identified by reviewing the bony windows on CT, however.