Adding CT perfusion scans to routine PET/CT offers critical new information about tumor viability that can improve staging and management noninvasively in patients with suspected lung cancer, according to a study from Italy.
Dr. Cristina Capraro and colleagues from the University of Milan-Biccoca said the imaging combination highlights the importance of necrosis in larger tumors, showing them to be less aggressive than their size and enhancement characteristics might suggest.
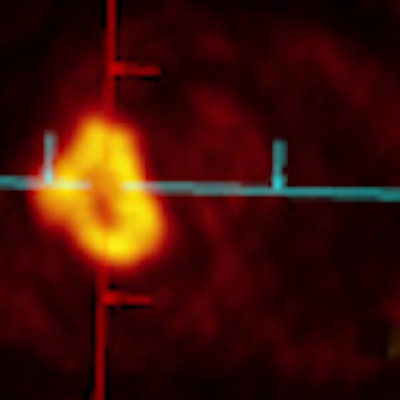
Lung cancer is the leading cancer killer, which means the choice of treatment, based on tumor stage, is the "central question in management," Capraro said. PET, with its high sensitivity for detecting mediastinal lymph nodes, is key to getting the staging right, and the limited anatomic information it provides can fortunately be overcome with the use of PET/CT, which provides both functional and anatomic data in a single exam, she said.
However, even though PET is good at evaluating tumor viability, "it doesn't provide any information about perfusion parameters," Capraro said. "Recently, there has been a gradual increase in the appeal of CT perfusion in oncology as the technique permits noninvasive quantification of the tumor angiogenesis that parallels the growth and spread of tumors and assessment of tumor aggressiveness," she said.
With that in mind, the study team aimed to assess the additional functional information and the relationship between perfusion measurements and glucose metabolism (SUVmax) obtained by incorporating CT perfusion study into a whole-body contrast-enhanced PET/CT protocol for lung cancer staging.
Capraro, Dr. Davide Ippolito, and colleagues prospectively examined 49 consecutive patients with biopsy-proven lung cancer (all but three had adenocarcinomas) who were referred for contrast-enhanced PET/CT staging. The imaging protocol included the following:
- Low-dose unenhanced whole-body PET/CT
- CT perfusion of the lung lesion to ensure optimal contrast for staging (120 kV and 80 mAs during injection of 50 mL of contrast at 5 mL/sec, followed by a second contrast bolus of 80 mL at 3 mL/sec after a 60-second delay)
- Whole-body contrast-enhanced CT
The total radiation dose was 4.3 mSv in all patients.
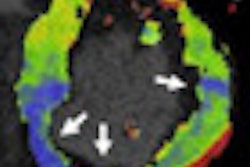
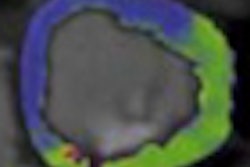
The CT perfusion data were used to calculate a range of tumor vascularity parameters in perfusion maps including blood flow, blood volume, and mean transit time. FDG uptake in PET imaging, expressed as SUVmax, was used as a metabolic indicator.
Armed with data from both protocols, the researchers compared quantitative and functional parameters and statistically analyzed them in relation to location, histology, and tumor size. The perfusion images were analyzed using commercially available software (Perfusion 3.0, Advantage, GE Healthcare), which generated quantitative maps of arterial perfusion.
The results showed insignificant differences in perfusion and metabolic parameters in relation to histological tumor type, as well as tumor location, she said.
However, significant perfusion differences were found "in relation to the size of the tumor -- in particular, lower perfusion parameters, especially blood volume and blood flow, except for mean transit time -- in tumors larger than 3 cm," she said (p < 0.005). Metabolic SUVmax was also found to be higher in neoplastic lesions larger than 3 cm.
"Comparing the metabolic and perfusion parameters in lesions larger than 3 cm, we found an interesting inverse relationship between blood volume and SUVmax and a significant direct relationship between mean transit time and SUVmax," she told delegates at the RSNA meeting at the end of last year.
Linear regression analysis showed the highest correlations between blood volume and SUVmax for the larger tumors. This finding can be explained by "the inability of new vascularization to support the fast growth of the tumor cells, seen as increasing enhancement at CT with development of necrotic areas of growth and necrosis within the tumor," she said.
The results may indicate that large tumors exhibit lower perfusion and higher metabolism in relation to their aggressiveness, showing that not only histological type but also size and the presence of necrosis determine the enhancement characteristics of lung carcinomas.
|
"In conclusion, we can say that necrosis is one of the most important factors associated with tumor aggressiveness, and perfusion parameters may have a potential role as indicators of prognosis and in monitoring antivascular chemotherapy," she said.
CT perfusion can be readily incorporated into PET/CT lung cancer protocols to provide a clearer picture of the biological characteristics of the tumor than shown by CT or PET/CT alone, she said.
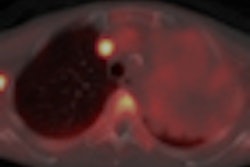
Editor's note: The image on our homepage is a fused PET/CT image that differentiates a large right upper lobe cancer from surrounding atelectasis. Image courtesy of Dr. Nigel Howarth, from the Institute of Radiology at the Clinique des Grangettes in Geneva, Switzerland.