CT angiography (CTA) has carved out a niche in heart imaging thanks to its ability to display cardiac morphology. But German researchers think it could have a role to play in functional imaging as well with the use of a dynamic CT perfusion technique they've developed that measures myocardial blood flow.
Dr. Konstantin Nikolaou, an associate professor of radiology at Ludwig Maximilian University of Munich, presented his findings on the dynamic stress perfusion CT technique at the recent International Society of Computed Tomography (ISCT) annual meeting in San Francisco.
He and his colleague Dr. Fabian Bamberg found it is feasible to perform myocardial perfusion CT under stress conditions, which increases the diagnostic accuracy in decision-making -- namely, whether a stenosis is functionally relevant or not. Ultimately, combining the technique with CT angiography could reduce false positives, and thus further diagnostic procedures.
The researchers performed CT-based dynamic stress myocardial perfusion imaging in both animals and humans with a Somatom Definition Flash scanner (Siemens Healthcare) in shuttle mode with the scanner's flash technique.
The researchers first tested the technique in an animal model, which enabled them to visualize how the technique worked under rest and stress conditions with a tightly controlled environment. The size of the stenosis could be controlled using a stent inserted into the left ascending artery that was always 3 mm in diameter; a balloon could be inflated precisely to larger diameters.
A 30-second scan was used with 50 cc of contrast at 5 mL/sec flow and adenosine administration. The scan produces 20 time points, creating a signal attenuation curve from which quantitative values can be derived.
The CT perfusion measurements were then compared with the gold standard for myocardial blood flow (MBF), in which fluorescent microspheres were injected into the left atrium of six pigs. MBF values were determined on a per-segment basis by spectrofluorometry after dissection of the myocardium.
In the animal model, the researchers found a total of 96 myocardial segments, 5% of which were excluded due to artifacts. They found that myocardial blood flow was dependent on the degree of stenosis under stress -- 50% stenosis under stress the blood flow was about 1.4 mL/g per minute; 75% stenosis, the rate was about 0.8 mL/g per minute, comparable with the CT-based measurement of myocardial blood flow.
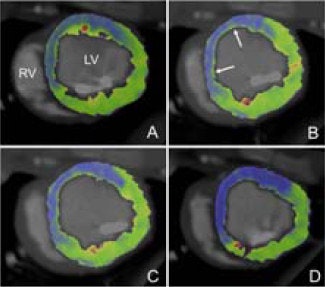 Myocardial blood flow at rest (A and C) and at stress (B and D) in the animal study. Image courtesy of Dr. Konstantin Nikolaou.
Myocardial blood flow at rest (A and C) and at stress (B and D) in the animal study. Image courtesy of Dr. Konstantin Nikolaou.Correlation in myocardial blood flow measurements with the CT perfusion and fluorescent microsphere techniques was good, with r = 0.71 (p = 0.003).
"What you're getting then is a real dynamic assessment of contrast-enhanced blood flow over time," Nikolaou said.
The protocol was similar for the 112 patients included in the study. After a topogram was performed, the researchers conducted a rest CTA with 60 cc of contrast and about 3 mSv of radiation dose. Then the CT perfusion was performed, with about 50 cc of contrast and adding another 9 mSv of radiation dose. In clinical practice, a normal CTA might preclude the CT perfusion study, Nikolaou said.
The prevalence of disease was rather high in the human patients, with 12% of segments and 56% of vessels with significant disease, although there were no infarct patients.
For comparison, Nikolaou and colleagues measured CTA's effectiveness in two ways: the first using an anatomically based definition of stenosis as luminal narrowing of greater than 50%, and the second based on hemodynamic criteria in which stenosis was considered to be a functional flow reserve of less than 75%.
With the anatomic measurement, CTA performed well, with sensitivity of 93.5%, specificity of 97.4%, and positive predictive value (PPV) of 82.9%. But using hemodynamic criteria, CTA's PPV fell to 48.6%, compared with 77.5% for estimated myocardial blood flow with CT perfusion. CT perfusion also recorded high sensitivity and specificity, at 91.2% and 98.2%, respectively. Using another yardstick, CT perfusion's area under the curve reached 0.90, compared with 0.75 for CTA alone.
"You can really take a lot of these false-positive diagnoses away," Nikolaou said.
Total radiation dose from the combined study was 10 to 12 mSv, a level that Nikolaou acknowledged was a bit on the high side but could be acceptable if enough relevant clinical information was derived. Also, he noted that CT perfusion can now be performed with iterative reconstruction, a protocol that was not available at the time of the study.
"This is something that has the potential to be translated into clinical routine. However, we still do not know where this tool would fit into our diagnostic strategies: Maybe a normal CTA prevents you from doing the perfusion scan, whereas in subjects with heavily calcified coronary plaque, CT-based perfusion imaging would be of great help," Nikolaou said. "I think from these two studies we can conclude indeed that combining CTA with the stress perfusion is first feasible and is really adding some incremental diagnostic value."
However, more studies are needed to confirm the findings, the researchers said.