Routine FDG-PET/CT imaging of patients with high-risk gram-positive bacteremia can reduce morbidity and mortality, and it does so in a cost-effective way, according to a study published in the Journal of Nuclear Medicine.
Dutch researchers concluded that additional in-hospital treatment for metastatic infectious foci is the primary contributor to the cost of $72,487 per prevented death, which is "well within the range" of cost efficiency.
Cost-effectiveness would further improve if patient treatment were based on abnormalities detected by FDG-PET/CT without the addition of other tests that contribute little information to a patient's outcome, the authors added.
The lead author of the study is Dr. Fidel Vos from the department of internal medicine and the Nijmegen Institute for Infection, Inflammation, and Immunity at Radboud University Nijmegen Medical Centre (JNM, October 7, 2011).
Bacteremia incidence
Vos and colleagues cited previous research to describe the severity of gram-positive bacteremia, which can result in high morbidity and a mortality rate of approximately 30%. Several European studies found that over the past few decades the incidence of Staphylococcus aureus bacteremia (SAB) has increased to 17 to 19 per 100,000 people, while both community- and hospital-acquired SAB increased to approximately 250 per 100,000 hospital discharges in the U.S.
Other studies estimated that infection added an average of $30,000 to $40,000 to healthcare costs in the 1990s, with those expenses likely greater today.
In an earlier study, Vos and colleagues showed that use of FDG-PET/CT to detect metastatic infectious foci in patients with SAB or Streptococcus spp. bacteremia reduced both relapse rates and mortality (JNM, August 1, 2010, Vol. 51:8, pp. 1234-1240).
During that research, they monitored costs associated with the use of FDG-PET/CT to evaluate the efficiency or cost-effectiveness in high-risk patients with gram-positive bacteremia.
"We hypothesized that early detection and treatment of metastatic foci would be cost-effective because fewer patients would be readmitted and treated for relapse of infection, or delayed cure," the authors wrote.
Study population
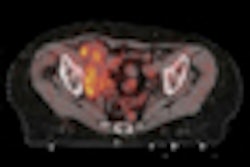
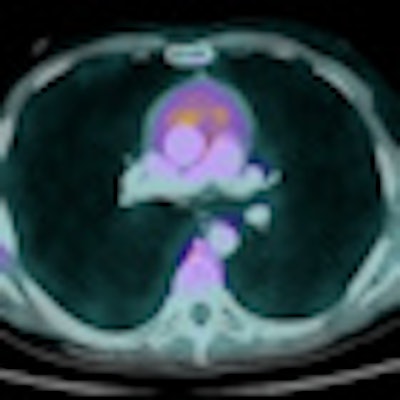
From 2005 to 2008, FDG-PET/CT was performed on 111 of 115 prospective study patients with gram-positive bacteremia in the first two weeks after their admission. The enrollees showed signs of at least one risk factor for developing metastatic infection foci, such as community acquisition, fever for more than 72 hours after initiation of treatment, or positive blood cultures more than 48 hours after treatment began. The group's mean age was 59 years.
Vos and colleagues also matched the patients' microorganism and risk profile for the presence of metastatic infectious foci with 230 control patients, who had a mean age of 58 years, in the same hospital in the four years preceding the prospective study. None of the 230 control subjects received an FDG-PET/CT scan.
Echocardiograms were given to patients in the FDG-PET/CT group, while subjects in the control group received echocardiograms only at the direction of an attending physician.
The authors noted that the incremental costs of FDG-PET/CT excluded patients with endocarditis because echocardiography is the standard imaging modality to detect the condition. Because of FDG uptake in the myocardium, FDG-PET/CT scans were not analyzed for possible endocarditis.
The length of stay was similar in both the FDG-PET/CT group (27 days) and the control group (28 days) with metastatic infection. In cases of no metastatic infection, the length of stay for patients in both groups was 14 days. Duration of treatment depended on whether a patient in either group had metastatic infectious foci.
Mortality at six months was used as the benchmark for patient outcome and was used to determine incremental cost-effectiveness.
A review of the 115 patients in the FDG-PET/CT group found an infection relapse rate of 2.6%, compared with 7.4% for the 230 patients in the control group. Overall mortality among the FDG-PET/CT group was 19%, compared with 32% for the control group.
Cost analysis
Mean total cost per patient in the FDG-PET/CT group was $31,710 (95% confidence interval [CI]: $25,954 to $37,465), compared with $22,255 in the control group (95% CI: $19,623 to $24,888), according to Vos and colleagues.
Incremental cost for the FDG-PET/CT group was $9,454 (95% CI: $3,963 to $14,947). Mean total cost of relapse of infection was $23,979 per patient for the three subjects in the FDG-PET/CT group who relapsed, compared with $20,679 per patient among the 17 patients who relapsed in the control group.
The largest contributor to incremental costs was admission days, with a mean cost of $6,631 per patient (95% CI: $1,449 to $11,814).
Endocarditis treatment
Given that patients in the FDG-PET/CT group received more FDG-PET/CT scans and echocardiograms, the number of patients with metastatic infectious foci increased, while the number of endocarditis diagnoses doubled.
Hence, treatment for endocarditis added to costs when echocardiography was figured into the analysis. By excluding all patients with endocarditis from the analysis, there was a decrease in incremental costs from $9,454 (95% CI: $3,963 to $14,947) to $5,277 (95% CI: $429 to $10,123).
"This figure cannot be translated into real costs contributed by FDG-PET/CT because in a subgroup of patients both endocarditis and other clinically relevant metastatic infectious foci requiring prolonged antibiotic treatment were present," the authors noted. "It shows, however, that both echocardiography and, in lesser part, FDG-PET/CT are cost drivers."
FDG-PET/CT "identified significantly more clinically relevant infectious foci, enabling early adjustment of treatment and a consequent decrease in mortality rates," Vos and colleagues concluded. "Associated costs resulted in a point-estimate of $72,487 per prevented death -- an investment that is well within the acceptable range."
The authors recommended that patients with high-risk gram-positive bacteremia have FDG-PET/CT scans for the early detection of metastatic infectious disease.