Building up an understanding of imaging mimics of female reproductive tract obstruction helps to guide anatomic localization and prevent interpretive errors, according to an article posted on 2 August in the European Journal of Radiology.
Making an accurate diagnosis in these cases may be challenging, particularly at initial ultrasound assessment, but it is critical because radiologic interpretation guides appropriate surgical management. MRI is particularly useful in lesion characterization and anatomic localization in difficult cases, noted radiology resident Dr. Monish Ahluwalia, abdominal radiologist and associate professor Dr. Andrew Chung, and colleagues at Queen's University, Kingston, Ontario, Canada.
“Cystic or necrotic lesions of the pelvis may mimic female reproductive tract obstruction,” they stated, adding that accurate diagnosis of the underlying cause facilitates appropriate and timely management. “Diagnosis of female reproductive tract obstruction relies on identifying the location of fluid distension.”
In their study, the researchers have highlighted a wide range of clinical scenarios that can arise. Four of these scenarios are outlined below.
OHVIRA syndrome
Obstructed hemivagina with ipsilateral renal agenesis (OHVIRA) syndrome, also known as Herlyn-Werner-Wunderlich syndrome, is a rare congenital Müllerian anomaly consisting of a triad of uterine didelphys, hemivaginal obstruction, and ipsilateral renal agenesis. This combination of anomalies can be explained by the relational development of the uterine and renal systems, they explained.
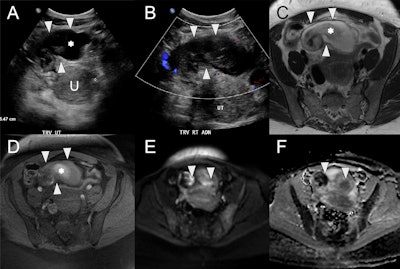
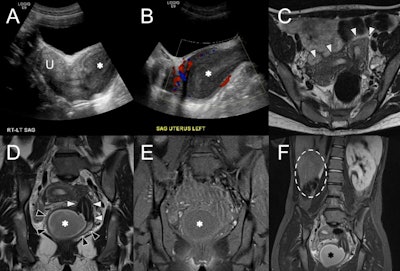 OHVIRA syndrome. (A) Sagittal ultrasound image at the level of the uterus (U) shows echogenic contents distending the vagina (asterisk) with (B) no color Doppler flow. (C) Axial T2w MRI shows two widely splayed uterine horns (white arrowheads). (D) Coronal T2w MRI demonstrates two separate cervices (white arrowheads) and vaginal cavities (black arrowheads) consistent with uterine didelphys. The right hemivagina is distended with fluid (asterisk), consistent with obstruction. (E) Coronal fat-suppressed T1w MRI at the same level shows low signal intensity of the vaginal contents (asterisk), suggestive of hydrocolpos. (F) Wide field-of-view fat-suppressed T2w MRI shows right renal agenesis (dashed line) ipsilateral to the side of vaginal obstruction (asterisk). All figures courtesy of Dr. Monish Ahluwalia, Dr. Andrew Chung, and EJR.
OHVIRA syndrome. (A) Sagittal ultrasound image at the level of the uterus (U) shows echogenic contents distending the vagina (asterisk) with (B) no color Doppler flow. (C) Axial T2w MRI shows two widely splayed uterine horns (white arrowheads). (D) Coronal T2w MRI demonstrates two separate cervices (white arrowheads) and vaginal cavities (black arrowheads) consistent with uterine didelphys. The right hemivagina is distended with fluid (asterisk), consistent with obstruction. (E) Coronal fat-suppressed T1w MRI at the same level shows low signal intensity of the vaginal contents (asterisk), suggestive of hydrocolpos. (F) Wide field-of-view fat-suppressed T2w MRI shows right renal agenesis (dashed line) ipsilateral to the side of vaginal obstruction (asterisk). All figures courtesy of Dr. Monish Ahluwalia, Dr. Andrew Chung, and EJR.
“Transabdominal and transvaginal ultrasound is the first-line imaging modality, which demonstrates uterine didelphys, echogenic hematocolpos or hematometrocolpos, and unilateral renal agenesis. There should be no colour Doppler flow in the vaginal contents to differentiate from a vascular mass. Care should be taken to appropriately delineate anatomic structures, as hematocolpos can be mistaken for a pelvic abscess or endometrioma,” the authors pointed out.
MRI allows for detailed delineation of uterine morphology and the continuity of each vaginal channel, in addition to the findings on ultrasound. Low signal on T1-weighted imaging (T1-WI) suggests hydrocolpos, while high signal indicates blood contents. CT may show similar findings, albeit with lower contrast resolution.
Cervical stenosis
Small volumes of endometrial fluid may be physiologic in premenopausal women. In postmenopausal women, the presence of physiologic fluid is controversial, though often benign if the patient is asymptomatic with normal endometrial thickness, they noted. In postmenopausal women, the differential for hydrometra includes cervical stenosis, cervical or endometrial carcinoma, and infection. “Larger volumes of hydrometra in premenopausal women could relate to congenital obstructions (imperforate hymen, transverse vaginal septum, vaginal or cervical atresia), acquired cervical obstruction due to instrumentation, prior radiation therapy, carcinoma, and pregnancy.”
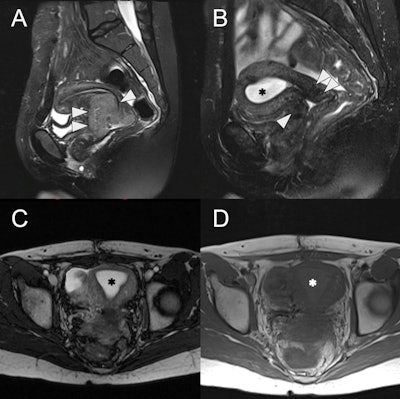 24-year-old female with radiation-induced cervical stenosis. (A) Pretreatment sagittal fat-suppressed T2w MRI of the uterus with a large intermediate to high signal intensity cervical mass (white arrowheads), FIGO stage IIB. (B) Sagittal fat-suppressed T2w MRI postchemoradiation showing marked regression of the tumor (white arrowheads) with reconstitution of the low signal intensity cervical stroma and no measurable residual mass. However, there is new distention of the endometrial cavity (asterisk) with high signal intensity. (C) Axial T2w MRI of the uterus with a distended endometrial cavity (asterisk), suggestive of obstruction. (D) Axial T1w MRI of the uterus shows mild hyperintensity (asterisk) of the endometrial fluid compared to myometrium, suggestive of hematometra
24-year-old female with radiation-induced cervical stenosis. (A) Pretreatment sagittal fat-suppressed T2w MRI of the uterus with a large intermediate to high signal intensity cervical mass (white arrowheads), FIGO stage IIB. (B) Sagittal fat-suppressed T2w MRI postchemoradiation showing marked regression of the tumor (white arrowheads) with reconstitution of the low signal intensity cervical stroma and no measurable residual mass. However, there is new distention of the endometrial cavity (asterisk) with high signal intensity. (C) Axial T2w MRI of the uterus with a distended endometrial cavity (asterisk), suggestive of obstruction. (D) Axial T1w MRI of the uterus shows mild hyperintensity (asterisk) of the endometrial fluid compared to myometrium, suggestive of hematometra
Cervical stenosis can be congenital, but is most commonly secondary to trauma, infection, malignancy, prior radiation, mass effect from adjacent Nabothian cysts or leiomyomas, or hormone-related changes. Hysteroscopy is the gold standard for diagnosis and treatment, and MRI is used to investigate for underlying causes, the researchers said.
Pyosalpinx
In cases of salpingitis, the uterine tubes become edematous with subsequent pyosalpinx. CT may demonstrate thickened uterine tubes (≥ 5mm) with enhancing walls and pelvic-free fluid, they wrote. Pyosalpinx appears as complex internal fluid or a complex cystic mass. Ultrasound may also demonstrate thickened tubes, but it also allows for the detection of hyperemia of the tube or ovary on Doppler imaging.
“A fluid-debris level indicates pyosalpinx. Spillage of pus into the peritoneal cavity allows for spread to the uterus and ovary, resulting in an inflammatory mass, sometimes known as a tubo-ovarian complex. Tubo-ovarian abscesses appear as multilocular septate masses with a thick enhancing wall on CT and as a complex cystic mass on ultrasound and MRI,” the authors stated.
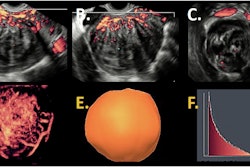
 Right pyosalpinx in a 42-year-old female with infectious symptoms and vaginal discharge postspontaneous abortion. (A) Axial ultrasound showing a distended tubular cystic structure (white arrowheads) anterior and to the right of the uterus (U, calipers) with internal echogenic debris (asterisk). (B) Ultrasound demonstrates no color Doppler flow within this structure (white arrowheads). (C) Axial T2w MRI of the uterus with a high signal intensity tubular structure (arrowheads) within the anterior pelvis, corresponding to the right uterine tube and containing intermediate to low signal debris (asterisk). (D) Axial fat-suppressed T1w MRI of the uterus shows high signal debris (asterisk) within the right uterine tube (white arrowheads). Axial high b-value diffusion-weighted image (E) and apparent diffusion coefficient map (F) demonstrate diffusion restriction of internal contents (white arrowheads), which, given the clinical context, is consistent with pus.
Right pyosalpinx in a 42-year-old female with infectious symptoms and vaginal discharge postspontaneous abortion. (A) Axial ultrasound showing a distended tubular cystic structure (white arrowheads) anterior and to the right of the uterus (U, calipers) with internal echogenic debris (asterisk). (B) Ultrasound demonstrates no color Doppler flow within this structure (white arrowheads). (C) Axial T2w MRI of the uterus with a high signal intensity tubular structure (arrowheads) within the anterior pelvis, corresponding to the right uterine tube and containing intermediate to low signal debris (asterisk). (D) Axial fat-suppressed T1w MRI of the uterus shows high signal debris (asterisk) within the right uterine tube (white arrowheads). Axial high b-value diffusion-weighted image (E) and apparent diffusion coefficient map (F) demonstrate diffusion restriction of internal contents (white arrowheads), which, given the clinical context, is consistent with pus.
MRI is the most sensitive modality to differentiate pyosalpinx (restriction on diffusion-weighted imaging), hematosalpinx (hyperintense on T1-WI), and hydrosalpinx (hypo- or isointense on T1-WI), they added. “CT and MRI also allow for diagnosis of additional complications such as septic thrombophlebitis and liver capsule adhesions (Fitz-Hugh-Curtis disease).”
Cystic/necrotic pelvic mass
Nonuterine masses such as nonuterine neoplasms and cystic lesions may mimic reproductive tract obstruction, and this is especially true if lesions are large, making localization challenging.
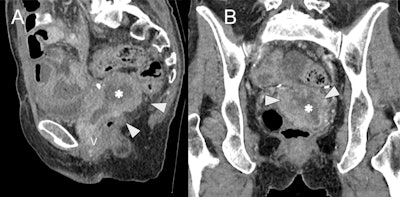 Cystic/necrotic pelvic mass mimicking hydro/hematometra in a 65-year-old female with recurrent ovarian cancer post total abdominal hysterectomy and bilateral salpingo-oophorectomy. Sagittal (A) and coronal (B) contrast-enhanced CT images demonstrate a soft tissue mass (white arrowheads) with central hypodensity, suggestive of cystic/necrotic component (asterisk). The mass is inseparable from the vaginal cuff (V) and mimics an obstructed, retroverted uterus, but instead represents local recurrence post hysterectomy.
Cystic/necrotic pelvic mass mimicking hydro/hematometra in a 65-year-old female with recurrent ovarian cancer post total abdominal hysterectomy and bilateral salpingo-oophorectomy. Sagittal (A) and coronal (B) contrast-enhanced CT images demonstrate a soft tissue mass (white arrowheads) with central hypodensity, suggestive of cystic/necrotic component (asterisk). The mass is inseparable from the vaginal cuff (V) and mimics an obstructed, retroverted uterus, but instead represents local recurrence post hysterectomy.
“Following ultrasonographic assessment, CT and MRI can be used to assist in characterization and localization. The vascular supply may assist in localization, for example, vascular supply from the gonadal vessels may suggest ovarian origin,” they said.
For more clinical cases and images, read the full EJR article here.