Molecular techniques continue to show immense promise, but to ensure their successful introduction, serious problems must be addressed, including the recruitment of well-trained staff and the maintenance of an appropriate regulatory framework.
The field of molecular imaging is experiencing an impressive period of innovation and growth. PET is becoming a leading tool to investigate changes in the living human body, thanks to the availability of reliable probes and the introduction of new and more specific radiopharmaceuticals, which hopefully can selectively image different pathways of a tumor's biology.
Modern PET often involves hybrid imaging: PET/CT sets the standard for functional imaging, and PET/MR systems are emerging from research apparatus to clinical tools.
The future, as always, is in our own hands. The availability of such sophisticated technologies, along with a multiprofessional setting, is going to change the environment of radiologists and nuclear medicine physicians. The near future will see a single specialist who is able to read multimodality molecular imaging and has a deep knowledge of the clinical setting in which images are obtained. Specialists will need to be experts in specific clinical fields, rather than in specific imaging modalities.
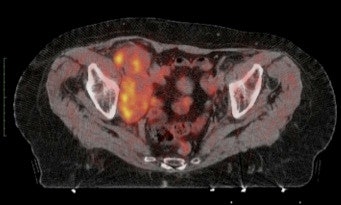 Example of the use of new radiopharmaceuticals: 11C-choline imaging of pathologic lymph nodes in advanced bladder cancer. Bulky disease in the right iliac region is easily recognized on PET/CT.
Example of the use of new radiopharmaceuticals: 11C-choline imaging of pathologic lymph nodes in advanced bladder cancer. Bulky disease in the right iliac region is easily recognized on PET/CT.Traditional nuclear medicine techniques -- the first tools to image molecular changes in the living body -- are evolving slowly compared with PET, and are considered mature imaging modalities, with well-defined diagnostic accuracy. FDG-PET, the well-known glucose analogue, is also considered a reliable tool for many applications: entering "FDG PET" into PubMed brings more than 40,000 items between 1975 and 2011. Thanks to FDG, many centers are already settled throughout the world and many others are on the way.
The growing number of nuclear medicine departments demands an increasing number of trained physicians, and this raises some problems. Doctors are difficult to recruit in many countries nowadays, and molecular imaging is not the most appealing discipline for many students. The fear of radiation exposure, the need to be familiar with many technical aspects, and the paucity of direct relationships with patients may be some of the causes. Doctors in nuclear medicine need specialized professionals to work with. Physicists, radiopharmacists, technologists, and nurses must be well trained and motivated to give the patient the best imaging and treatment available.
New ideas and young minds are essential for the development of any discipline. Making molecular imaging appealing for students and young scientists should be the first priority over the next few years. We have to develop a strategy for making the discipline more attractive. We must convince younger colleagues that molecular imaging is a stimulating discipline that can provide answers to clinicians like no other technique can do, and has a significant impact on patient management. Similar strategies should be developed to attract young physicists, radiopharmacists, technologists, and nurses.
One of the best ways to attract young people to a research field is to make its characteristics visible and underline its strength in improving healthcare. Recent developments in molecular imaging fit well with this goal. Besides FDG-PET, more advanced techniques are entering the clinical arena. Evaluation of response in lymphoma and solid tumors, along with the integration of PET images in radiation therapy planning, are just a couple of strong examples of new applications of FDG PET/CT in oncology. Infection imaging is another emerging field, and improvements are being made in diagnosing infectious diseases, in which other imaging techniques have been of little value.
The real frontier is the introduction of new radiopharmaceuticals in clinical practice. New and specific probes are already available in academic centers: choline for prostate cancer and primary liver carcinoma, methionine for brain tumors, somatostatin analogue peptides for neuroendocrine tumors, fluoride for bone imaging, and fluorothymidine for cell proliferation. These are just some examples of the great potential of PET/CT imaging in oncology using radiopharmaceuticals. New radiopharmaceuticals are already in the pipeline and are going to be able to characterize certain aspects of different tumors, allowing the treatment to be tailored to the individual patient.
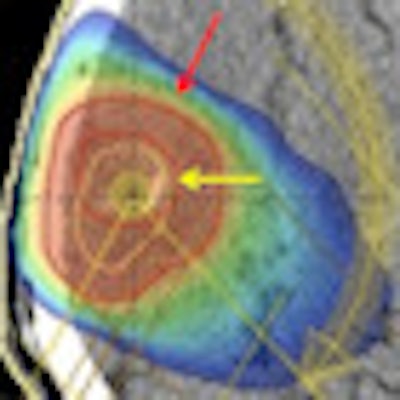
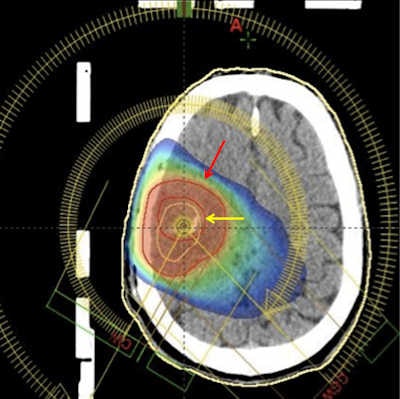 Radiation treatment planning of a brain tumor. Adding 11C-methionine PET increases the tumor volume (red arrow) when compared to the blood brain disruption as imaged by gadolinium-enhanced MRI (yellow arrow).
Radiation treatment planning of a brain tumor. Adding 11C-methionine PET increases the tumor volume (red arrow) when compared to the blood brain disruption as imaged by gadolinium-enhanced MRI (yellow arrow).In the next five years, we will likely see another technetium shortage. Although dedicated investments and new production techniques are going to reduce the impact of the next molybdenum production crisis, the global economic crisis will have a negative impact on the availability of the widely used radionuclide for single-photon molecular imaging. The reduced availability of funding for renovation or construction of production facilities, the increased costs of transportation, and the reduction in research funding will contribute to the difficulties in keeping the availability of technetium at the requested level for worldwide supplies. This is going to be another driving force to the use of PET techniques, as an alternative to single-photon imaging.
Excessive controls
Avoiding the growth of excessive bureaucracy and regulations will be another important challenge over the coming years. Many advantages have come from the application of strict procedures and safety controls, but we are all aware that in many cases the amount of paperwork required for an activity has neither justification nor any relation to the activity itself. We must evolve, and evolution requires the ability to change rapidly.
Radiopharmaceuticals used in PET imaging are a clear example of the limitations that can be imposed by bureaucracy on research and healthcare. In many cases, a patient's safety could be ensured with less strict requirements than those imposed for pharmaceuticals products used for therapy, not for imaging. We need rules that can be updated in real-time -- with essential and clear structure -- designed to help and facilitate the work of scientists and clinicians, not the work of bureaucrats.
Standardization of imaging procedures is a must. We need strong procedures to ensure that PET images produced in different centers with different scanners can be safely compared. Standards for quality control and quality assurance procedures have to be issued by scientific societies able to give accreditation to centers following the quality programs. This will make the techniques trusted and useful for clinicians and patients, increasing the level of quality of all centers able to get the accreditation.
Continuing education on clinical activities, not only on imaging modalities, and constructive competition between centers will be the final requirements for the "molecular imager."
The next few years will be evolutionary for many aspects of the world as we know it. Molecular imaging has to be evolutionary as well in order to keep on growing.
Dr. Arturo Chiti is the director of the nuclear medicine department at the Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Humanitas in Milan and the committees coordinator of the European Association of Nuclear Medicine. Dr. Margarita Kirienko is a nuclear medicine physician in the Centre of Molecular Bioimaging at the University of Milan-Bicocca in Monza, Italy.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.




















