
VIENNA - Advances in molecular imaging promise to make it realistic to identify differences in response of cancer cells to a specific treatment, and this information will eventually be used to better adapt therapies to a patient's specific needs. The paradigm is becoming "image-drug-image" and then determination of whether the patient continues a therapy or switches, believes Dr. Ferdia Gallagher, honorary consultant radiologist and Cancer Research UK clinician scientist fellow at the University of Cambridge in the U.K.
"In the future, we will be using new techniques with MRI to improve patient outcomes in oncology, which will be more sensitive and specific in determining whether patients are on the correct therapy," said Gallagher, who will discuss molecular imaging with an emphasis on hyperpolarization, a technique also known as hyperpolarized carbon-13 MRI, during this afternoon's refresher course.
 In the future, new MRI techniques will be used to improve patient outcomes in oncology, according to Dr. Ferdia Gallagher.
In the future, new MRI techniques will be used to improve patient outcomes in oncology, according to Dr. Ferdia Gallagher.
Hyperpolarized carbon MRI is a technique that Cambridge-based scientists have been investigating in animals for several years. It detects cancer and early response to treatment. The first human trials took place in the U.S. in 2011, and the Cambridge group has recently acquired equipment with the aim of starting imaging trials in cancer patients.
Unlike fluorodeoxyglucose (FDG)-PET imaging, which shows the accumulation of a labeled substrate, hyperpolarization stands out because MRI can differentiate multiple metabolites from each other. PET imaging only provides a single, less defined output.
"The beauty of hyperpolarization is that it massively increases the signals of MRI by 10- to 100,000-fold. This allows us to see metabolism, which we have previously been unable to measure," noted Gallagher, who stressed that hyperpolarization will not replace other imaging modalities but is likely to complement existing anatomical imaging with CT, MR, and existing metabolic information.
Initially, the Cambridge group hopes to use the technique on patients with lymphoma, breast cancer, and glioma to determine response to chemotherapy or radiotherapy.
"With conventional CT, a therapy response can be seen after many weeks and if the patient fails to respond then we switch therapies. But in waiting for the tumor to grow, we might miss the boat. We want to determine if the treatment is working within hours or days," he said. "The earlier the intervention, the better."
Acknowledging the rapid advances in biological understanding of the cell, Gallagher thinks molecular imaging has huge scope in this new era of medicine. Diagnostics and therapy increasingly take a molecular approach, and now disease diagnosis can be stratified histologically and treatments are often highly targeted, then imaging needs to parallel this.
"Imaging needs to move in the direction that other aspects of medicine are moving in order to complement that," he commented.
Today's session on molecular imaging in oncology will discuss the growing toolbox of molecular imaging agents for cancer. In addition to hyperpolarization, which promises to image cancer cell activity on a new level by providing a rapid measure of patient treatment response, various PET tracers will be addressed.
 Europe is leading the world in the development of PET tracers for oncology, according to Dr. Peter Choyke.
Europe is leading the world in the development of PET tracers for oncology, according to Dr. Peter Choyke.
Standing up for PET imaging will be Dr. Peter Choyke, head of the imaging section of the Molecular Imaging Program at the National Cancer Institute in Bethesda, Maryland, U.S., who reckons the range of new PET agents can cover all the major hallmarks of cancer. PET is valued for its high sensitivity, which is essential for viewing the small number of receptors on the surface of cancer cells. In fact, PET has around a tenfold higher sensitivity than the next most sensitive modality, SPECT, as well as having better resolution, he noted.
Discussing the various PET agents, Choyke said FDG-PET is probably the most widely used agent that detects cancer cells by radiolabeling glucose. But he pointed out that while FDG has revolutionized the diagnosis and treatment of cancer, it is relatively nonspecific and other agents are needed to look at other features of cancer, such as cell proliferation to differentiate between cancer and inflammation, which is often present in cancer after therapy.
Like Gallagher, Choyke is keen to improve the measurement of cancer cell response to the many targeted therapies available.
"By noninvasively measuring levels of specific targets or receptors in cancer cells, clinicians will be able to predict better which patients will respond to these expensive therapies," he said.
Other PET agents that will be discussed by Choyke and that allow tracking of cancer cell activity include sodium fluoride, fluoro-L-thymidine (FLT), fluorocholine (FCH), carbon-11 (C-11) choline, and fluciclatide. For instance, a sodium fluoride scan can pick up bone metastases earlier than conventional bone scans.
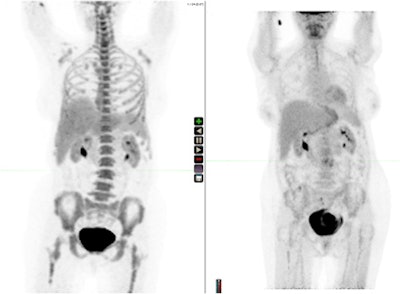 A fluoro-L-thymidine scan (left) and a fluorodeoxyglucose PET scan (right) of the same patient. Images courtesy of Dr. Peter Choyke.
A fluoro-L-thymidine scan (left) and a fluorodeoxyglucose PET scan (right) of the same patient. Images courtesy of Dr. Peter Choyke."It's very useful since it can detect metastatic disease earlier and may replace conventional bone scans in the near future for many indications," said Choyke, adding that in many respects sodium fluoride is a "dumb" agent because it simply reflects bone metabolism and is not a molecularly targeted agent.
FLT is more highly targeted and reflects cell proliferation. Since inflammatory masses are not highly proliferative, FLT scans can be used to distinguish between tumors and inflammatory masses in treated patients in which the FDG scan is positive, he remarked.
FCH and C-11 choline are two other agents targeted to prostate cancers. Choline is a phospholipid precursor that is taken up in higher amounts in prostate cancer cells than in normal cells. It can be used to detect prostate cancer that is invisible on FDG but is nonetheless recurring after treatment for prostate cancer.
Finally, an agent such as fluciclatide targets tumors with high levels of angiogenesis, and thus the agent may predict which tumors will respond to antiangiogenic therapies. Choyke reported that a study is ongoing to determine whether fluciclatide uptake is predictive of response to therapy.
In conclusion, he pointed out that the pace of clinical trials with these agents is restricted by costs and this has limited the diffusion of the technology into clinical medicine. For a variety of reasons, Europe is leading the world in the development of these agents, while relatively few centers are actively pursuing new PET imaging agents for cancer in the U.S., he said.
Originally published in ECR Today on 7 March 2013.
Copyright © 2013 European Society of Radiology



















