For patients with high-grade glioma brain tumors, radiotherapy, chemotherapy, and surgery remain palliative treatment options, driving research for a cure. Toward this goal, researchers in Australia have combined x-rays, chemotherapy, and a radiosensitizing drug in vitro to more than double tumor cell death compared with a radiation-only control. The combination selectively targets tumor cells and has the potential to reduce side effects in patients.
"We were extremely pleased with these results that are unprecedented in vitro on an extremely aggressive glioma cell line," said study co-author Stéphanie Corde, PhD, medical physicist at the Centre of Medical Radiation Physics at the University of Wollongong and Prince of Wales Hospital in Sydney. "We demonstrated that by mixing existing therapies together we could achieve a lot more than any of these therapies alone."
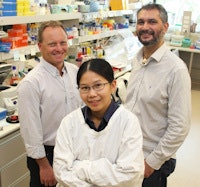 Study co-authors, left to right: Michael Lerch, Sianne Oktaria, and Moeava Tehei from Illawara Health and Medical Research Institute (IHMRI), University of Wollongong.
Study co-authors, left to right: Michael Lerch, Sianne Oktaria, and Moeava Tehei from Illawara Health and Medical Research Institute (IHMRI), University of Wollongong.Corde, first author Sianne Oktaria, and colleagues from the university's interdisciplinary targeted nano therapies group, tested the commonly used chemotherapy drug methotrexate (MTX) in their study. A folate analog, it preferentially accumulates in brain tumor cells as they overexpress cell surface receptors of the molecule. Once in place, the drug inhibits the production of tetrahydrofolate, which in turn inhibits the synthesis of thymidine, a key compound required for tumor cell division (Physics in Medicine and Biology, 25 September 2015, Vol. 60:20, pp. 7847-7859).
Upon administration, the radiosensitizer bromodeoxyuridine (BrUdR) incorporates itself into tumor cell DNA as an analog and competitor of thymidine. Upon irradiation with kilovoltage x-rays, bromine atoms in the BrUdR molecules interact predominantly by the photoelectric effect, due to its high atomic number. The resulting low energy and high linear energy transfer (LET) secondary electrons have a short range, producing highly localized damage.
In vitro investigations
The researchers tested the combination therapy in radioresistant 9L rat gliosarcoma cells cultured in flasks. The cells were incubated with MTX and/or BrUdR over two cell doubling times and irradiated with x-ray energies from 50 kVp to 10 MV by an orthovoltage unit and linac. Cell populations treated with the two-drug combination showed greater cell killing than those treated with radiation alone. The experiments also revealed the enhancement in tumor cell killing had a strong dependence on photon energy. A combination of the two drugs and a 125 kVp x-ray beam demonstrated the biggest radiobiological effect for a given dose (p < 0.0003).
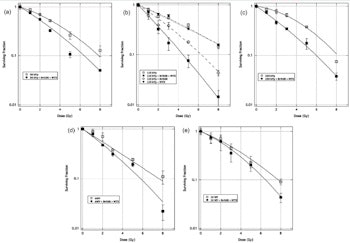
For each x-ray energy tested, the researchers observed an increase in cell killing with the use of both MTX and BrUdR drugs.
Using the 125 kVp beam, the combination therapy needed 2.3 times less dose than radiation alone to kill 90% of tumor cells in a given population. In comparison, the next most effective x-ray energy was a 6 MV beam, where the enhancement in cell killing was by a factor of 1.4.
The physical efficacy of the 125 kVp beam in combination with the two drugs is attributable to the bromine atom in BrUDr. Peaking at 40 keV, the element's mass energy absorption is close to the 46 keV effective energy of the beam, maximizing the likelihood of interaction between the two. Cell survival data provided evidence that MTX amplifies the biological impact of the radiation-BrUdR combination by limiting the repair of damaged DNA in the tumor cells.
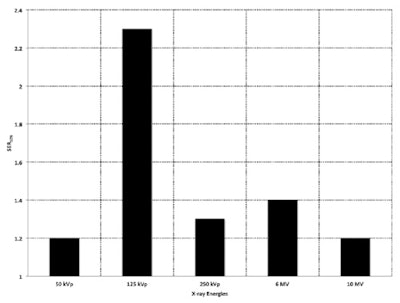 The researchers observed the greatest enhancement in cell killing over a radiation-only control using the two drugs with a 125 kVp x-ray beam. Beam energies were compared using a sensitivity enhancement ratio, SER10%, the ratio of doses needed to achieve the same radiobiological effect of 10% survival.
The researchers observed the greatest enhancement in cell killing over a radiation-only control using the two drugs with a 125 kVp x-ray beam. Beam energies were compared using a sensitivity enhancement ratio, SER10%, the ratio of doses needed to achieve the same radiobiological effect of 10% survival.A combination of BrUdR and radiation was less effective than the three-pronged approach. It achieved the same radiobiological effect with 1.6 times less dose than the radiation only control, using the 125 kVp beam. A combination of MTX and radiation, omitting the radiosensitizer, provided no advantage over radiation alone.
Subject to further research, Corde envisages clinical treatments with an external kilovoltage x-ray beam, using energies slightly higher than the optimal energy confirmed by the study to improve penetration of the brain. "A tunable quasi-monochromatic x-ray source would be ideal for the proposed scenario, with photon energies ranging from 30 to 150 keV," Corde said. As a next step toward clinical translation, the group plans to test the combination therapy in vivo in small-animal models within the next year.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.