Prostate-specific membrane antigen (PSMA) PET/CT has set a new benchmark in a phase II trial for primary staging of prostate cancer by substantially improving the detection of metastatic disease, a team in Germany has reported.
Among 137 patients with low-, intermediate-, and high-risk disease, PSMA-PET/CT altered management plans in 34% of patients, noted lead author Dr. Philipp Krausewitz, of University Hospital Bonn, and colleagues.
“These findings underscore the potential of PSMA-PET/CT to guide early, individualized treatment strategies,” the group wrote. The study was published on 6 November in the Journal of Nuclear Medicine.
Since its approval in 2020 for staging advanced prostate cancer, gallium-68 (Ga-68) PSMA-11 PET/CT has had a significant clinical impact. It is used in men after they have been diagnosed who are at high risk for nodal or metastatic disease because it offers superior detection of metastases compared with conventional imaging modalities, the authors explained.
However, given PSMA-PET/CT’s high accuracy, researchers are exploring its potential role in initial cancer detection and whether it can guide localized treatment.
To that end, between 2021 and 2023, Krausewitz and colleagues conducted a prospective, phase 2 interventional trial. They enrolled 230 men with suspected prostate cancer who had not yet had biopsies or previous imaging. Participants underwent PSMA-PET/CT and multiparametric MRI (standard of care) prior to targeted ultrasound fusion and systematic biopsies.
Next, expert teams of clinicians independently reviewed the histopathology and imaging data from either the multiparametric MRI (mpMRI) or the combined mpMRI plus PSMA-PET/CT pathway and formulated treatment plans accordingly.
According to the results, 137 of the 230 men had prostate cancer: 9% low-, 35% intermediate-, and 15% high-risk disease. Among these, PSMA-PET/CT altered management plans in 34% of patients, primarily modifying local treatment strategies, including lymph node dissection (16%), a nerve-sparing procedure (18%), and radiation field adjustments (28%).
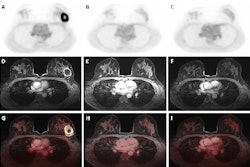
 Axial views of exemplary case studies in which additional PSMA PET/CT changed prostate cancer (PCa) management. (A–D) A 68-year-old man with isolated PSA elevation had no tumor-suggestive findings on mpMRI (A and B), but they were high suggestive of PCa on PSMA-PET/CT (C). After radical prostatectomy, 22-mm index tumor identified on PSMA- PET/CT was confirmed with Gleason score of 7a (D). Reviewers without PSMA-PET/CT information (MRI-only pathway) recommended continued PCa screening, whereas reviewers with PSMA PET/CT knowledge suggested active treatment. (E–H) A 72-year-old man with PSA of 9.1 ng/mL and suggestive prostate palpation had highly suggestive PCa lesion on both mpMRI (E and F) and PSMA-PET/CT (G). PSMA-PET/CT also detected two small osseous metastases in left ilium (H) and sacrum. Management recommendations varied: local therapy (surgery or radiation) without PSMA PET/CT knowledge versus androgen deprivation therapy and radiation for primary tumor and metastases with PSMA-PET/CT knowledge.Journal of Nuclear Medicine
Axial views of exemplary case studies in which additional PSMA PET/CT changed prostate cancer (PCa) management. (A–D) A 68-year-old man with isolated PSA elevation had no tumor-suggestive findings on mpMRI (A and B), but they were high suggestive of PCa on PSMA-PET/CT (C). After radical prostatectomy, 22-mm index tumor identified on PSMA- PET/CT was confirmed with Gleason score of 7a (D). Reviewers without PSMA-PET/CT information (MRI-only pathway) recommended continued PCa screening, whereas reviewers with PSMA PET/CT knowledge suggested active treatment. (E–H) A 72-year-old man with PSA of 9.1 ng/mL and suggestive prostate palpation had highly suggestive PCa lesion on both mpMRI (E and F) and PSMA-PET/CT (G). PSMA-PET/CT also detected two small osseous metastases in left ilium (H) and sacrum. Management recommendations varied: local therapy (surgery or radiation) without PSMA PET/CT knowledge versus androgen deprivation therapy and radiation for primary tumor and metastases with PSMA-PET/CT knowledge.Journal of Nuclear Medicine
In addition, 2% of patients initiated active treatment, 5% received adjunctive hormone therapy, and 7% underwent metastasis-directed therapy. The researchers noted that upfront PSMA-PET/CT prompted treatment intensification at comparable rates in both intermediate-risk and high-risk disease with high interrater agreement (Cohen's kappa coefficient, 0.71).
“Our findings confirm that PSMA-PET/CT complements mpMRI by improving the detection of localized [prostate cancer] at biopsy and indicate that PSMA-PET/CT alone can match mpMRI in guiding targeted biopsy in biopsy-naïve men,” the group wrote.
Ultimately, the integration of PSMA-PET/CT may increase costs, examination times, and diagnostic workload, while limited access to the method and a shortage of trained professionals remain significant barriers to widespread implementation, the authors noted.
Nonetheless, the trial met its primary objective, which was to demonstrate that upfront PSMA- PET/CT has a significant impact on treatment decision-making based on imaging and biopsy-derived information.
“Future studies should determine whether this approach translates into improved long-term oncologic and functional outcomes,” the researchers concluded.
The full study is available here.