Fetal cardiovascular MRI provides clinically useful information about congenital heart defects when echocardiography results are inconclusive, changing treatment/management plans in more than 80% of cases, according to a study published online on 29 March in JAMA Network Open.
The results suggest that cardiovascular MRI could improve treatment and management plans for infants with congenital heart defects and counseling for their parents, wrote a team led by Dr. Daniel Salehi of Lund University in Sweden.
"In [our] cohort study of 31 fetuses referred for fetal cardiovascular magnetic resonance imaging, additional clinically useful information regarding cardiovascular anatomy and function was obtained in 84% of referred cases, covering a wide spectrum of congenital heart defects," the group noted. "This information affected choice of mode of delivery, planning of early postnatal care, and parental counseling."
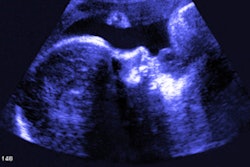
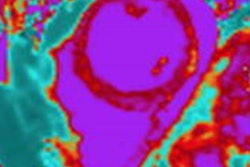
 Evaluation of atrial restriction in a fetus with hypoplastic left heart syndrome. Fetal echocardiography could not visualize the atrial cavity or Doppler flow across the atrial septum due to poor acoustic windows (A). Fetal cardiovascular MR showed a large interatrial communication, indicated by the asterisk, and no nutmeg pattern (B). Therefore, the risk of restrictive atrial septum was considered low (albeit a membrane could not be ruled out), and the fetus was planned for a vaginal delivery without cardiac catheterization laboratory on standby. Contrast and brightness in the cardiovascular MR image have been optimized for printing. All figures courtesy of JAMA Network Open.
Evaluation of atrial restriction in a fetus with hypoplastic left heart syndrome. Fetal echocardiography could not visualize the atrial cavity or Doppler flow across the atrial septum due to poor acoustic windows (A). Fetal cardiovascular MR showed a large interatrial communication, indicated by the asterisk, and no nutmeg pattern (B). Therefore, the risk of restrictive atrial septum was considered low (albeit a membrane could not be ruled out), and the fetus was planned for a vaginal delivery without cardiac catheterization laboratory on standby. Contrast and brightness in the cardiovascular MR image have been optimized for printing. All figures courtesy of JAMA Network Open.Although congenital heart defects affect only 1% of children, they account for 30% of infant mortality caused by from-birth anomalies. Complex defects that need intervention in the child's first year make up 25% of all cases, the group noted.
Congenital heart defects are typically identified in utero by echocardiography, but sometimes that modality proves inconclusive due to inadequate acoustic windows. In recent years researchers have developed an MR-compatible Doppler ultrasound device that allows for the acquisition of high-resolution fetal cardiovascular MR (CMR) images without postprocessing.
Salehi and colleagues sought to investigate the efficacy of fetal CMR after inconclusive echocardiography, as well as whether its use resulted in any patient management or parental counseling changes. The team conducted a study of 31 fetuses referred for cardiovascular MRI at Skåne University Hospital in Lund between January 2017 and June 2020; fetuses had a median gestational age of 36 weeks.
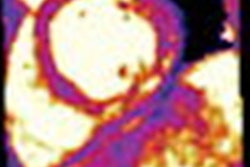
 Basic assessment in a fetus with risk factors for cardiac malformation and a very poor acoustic window. The fetal heart and vessels were not visible at all during fetal echocardiography, due to mother having obesity (A). Fetal cardiovascular MRI showed normal-sized ventricles with normal systolic function and at least one normal pulmonary vein (PV) without obvious direct or indirect signs of aberrant pulmonary veins (B), superior venae cavae (SVC) and inferior venae cavae (IVC) and normal ascending aorta (Ao) (C), and normal main pulmonary artery (MPA) (D). This information ruled out major congenital heart disease, and delivery was planned at the hospital closest to the patient's home. A nonurgent postnatal echocardiography examination was performed before discharge, which showed a normal cardiovascular anatomy.
Basic assessment in a fetus with risk factors for cardiac malformation and a very poor acoustic window. The fetal heart and vessels were not visible at all during fetal echocardiography, due to mother having obesity (A). Fetal cardiovascular MRI showed normal-sized ventricles with normal systolic function and at least one normal pulmonary vein (PV) without obvious direct or indirect signs of aberrant pulmonary veins (B), superior venae cavae (SVC) and inferior venae cavae (IVC) and normal ascending aorta (Ao) (C), and normal main pulmonary artery (MPA) (D). This information ruled out major congenital heart disease, and delivery was planned at the hospital closest to the patient's home. A nonurgent postnatal echocardiography examination was performed before discharge, which showed a normal cardiovascular anatomy.The authors found that cardiovascular MRI affected patient management and/or parental counseling in 84% of the cases, and added useful diagnostic and/or management information to the following situations:
- 80% of fetuses with aortic arch anatomy, including signs of coarctation
- 87% of fetuses with univentricular versus biventricular outcome in borderline left ventricle, unbalanced atrioventricular septal defect, and pulmonary atresia with intact ventricular septum
- 75% of fetuses with hypoplastic left heart syndrome
- 68% of parental counseling cases
"These findings suggest that fetal CMR has the potential to affect clinical decision-making in challenging cases of congenital heart defects with inconclusive data from echocardiography," the team concluded.
Yes, fetal CMR shows promise for diagnosing prenatal congenital heart disease, but don't throw out echocardiography, cautioned Dr. Bhawna Arya of Seattle Children's Hospital, U.S., in an accompanying commentary.
"The utility of fetal CMR is limited to late gestations because larger fetal size facilitates static MR imaging. ... Fetal echocardiography, in contrast, can identify significant congenital heart disease as early as 12 weeks gestation," Arya wrote.
"Although fetal CMR provides an appealing opportunity for advanced, late gestation imaging, fetal echocardiography remains the gold standard for early and accurate in utero diagnosis and monitoring of congenital heart disease and other fetal cardiovascular diseases," she concluded.