Advanced imaging is playing a key role in diagnosing cardiac manifestations in COVID-19 patients, including myocarditis, acute coronary syndrome, and thromboembolic events, researchers from Rome have reported. They've shared three new clinical cases.
Cardiac involvement is common in COVID-19 patients, leading to a morbidity/mortality increase, noted Dr. Federica Catapano and colleagues from the department of radiology at Sapienza University of Rome in an article posted on 24 February by Insights into Imaging. Radiologists should be aware of the wide and heterogeneous spectrum of cardiovascular complications in COVID-19 and optimum use of advanced imaging tools that may be used to drive therapeutic approach and stratify patients' prognosis.
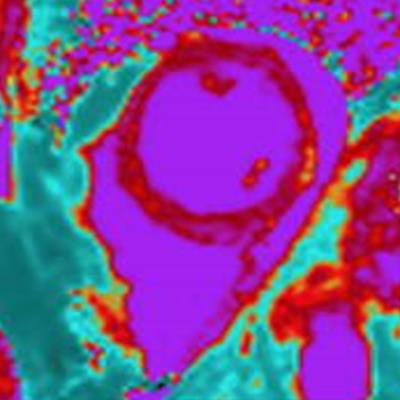
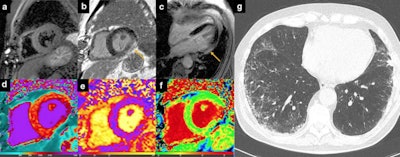 Myocarditis. 51-year-old man hospitalized for COVID‐19 pneumonia and sudden onset of tachyarrhythmias. short tau inversion recovery images revealed no edema (a), although late gadolinium enhancement (LGE) was evident on inferolateral segments of basal-mid planes with a subepicardial pattern of distribution (b, c: orange arrows) and native T1 was increased on LGE + segments (d). T2 mapping sequences revealed the presence of edema on inferolateral segments of mid-ventricular planes (e). Extracellular volume confirmed those findings with implemented values on inferolateral wall (f). Chest CT showed ground glass opacity predominantly distributed on inferior lobes with a peripheral distribution (g). All images courtesy of Dr. Federica Catapano and Prof. Marco Francone and Insights into Imaging.
Myocarditis. 51-year-old man hospitalized for COVID‐19 pneumonia and sudden onset of tachyarrhythmias. short tau inversion recovery images revealed no edema (a), although late gadolinium enhancement (LGE) was evident on inferolateral segments of basal-mid planes with a subepicardial pattern of distribution (b, c: orange arrows) and native T1 was increased on LGE + segments (d). T2 mapping sequences revealed the presence of edema on inferolateral segments of mid-ventricular planes (e). Extracellular volume confirmed those findings with implemented values on inferolateral wall (f). Chest CT showed ground glass opacity predominantly distributed on inferior lobes with a peripheral distribution (g). All images courtesy of Dr. Federica Catapano and Prof. Marco Francone and Insights into Imaging."Rational utilization of advanced cardiac imaging services in COVID-19 should serve to avoid or at least minimize the unnecessary use of invasive, potentially contagious and time-consuming procedures like cardiac catheterization or transesophageal echocardiography and to speed-up diagnostic pathways," they said.
While bedside echocardiography remains a first-line and ease-of-use diagnostic tool, appropriate use of second-line techniques, such as cardiac CT and cardiovascular MRI, allows the reliable exclusion of coronary artery disease together with the characterization of underlying pathological substrate.
"A progressive shift from acute to chronic cardiovascular damage is not uncommon, even in apparently healed patients, and includes conditions like chronic thromboembolic pulmonary hypertension, recurrent arrhythmias, and progression to dilated cardiomyopathy. Accordingly, careful follow-up of these patients should be ordered in the convalescent stage," the authors recommended.
What to know about pericarditis
Pericarditis is not a common complication in COVID-19, but it should be promptly considered in patients with chest pain, ST elevation on electrocardiogram, and a normal coronary angiogram. A misdiagnosis can produce life-threatening consequences, such as cardiac tamponade.
Despite the fact that CT and cardiac MRI are not included in the diagnostic criteria for pericarditis, these imaging modalities can provide supportive findings and are strongly recommended as second-level testing for diagnostic workup of the pathology, according to the authors. The hallmark of cardiac MRI in acute pericarditis includes the combination of diffusely edematous and enhancing pericardial layers with a variable amount of effusion, as shown in the figure below. MRI may serve not only to confirm the diagnosis but also to rule out alternative overlapped diagnoses such as myocarditis or pulmonary embolism.
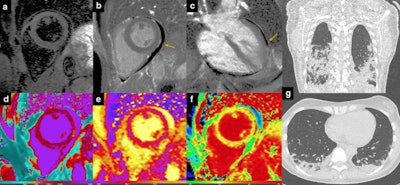 Pericarditis. 36-year-old in-hospital COVID-19 patient with chest discomfort and evidence of pericardial effusion at bedside echocardiography. In (a), there is evidence of slight hyperintensity of the pericardial layers, with no myocardial edema. LGE sequences confirm presence of pericardial layers enhancement and moderate pericardial effusion (b, c: orange arrows). Native T1 values were mildly increased (d) as well as T2 mapping (e) and extracellular volume values (f). Coronal and axial chest CT revealed peripheral posterior areas of parenchymal consolidation (g).
Pericarditis. 36-year-old in-hospital COVID-19 patient with chest discomfort and evidence of pericardial effusion at bedside echocardiography. In (a), there is evidence of slight hyperintensity of the pericardial layers, with no myocardial edema. LGE sequences confirm presence of pericardial layers enhancement and moderate pericardial effusion (b, c: orange arrows). Native T1 values were mildly increased (d) as well as T2 mapping (e) and extracellular volume values (f). Coronal and axial chest CT revealed peripheral posterior areas of parenchymal consolidation (g).Additionally, in the COVID-19 era, conventional echocardiography (i.e., not bedside) is potentially underused due to an increased infection risk for healthcare providers during the examination, they added.
Looking to the future
The Sapienza group started cardiovascular imaging studies in COVID-19 patients immediately after the first outbreak in Italy in early March 2020, having realized that the viral infection had a peculiar tropism for the cardiovascular system.
The researchers are keen to understand the role of imaging in the post-COVID-19 setting because they have seen that some apparently healed patients are potentially exposed to the sequelae of SARS-CoV2 disease, including dilated cardiomyopathy (particularly postmyocarditis), chronic heart failure, and postembolic pulmonary hypertension.
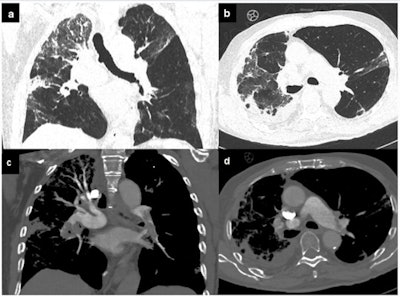 Pulmonary embolism. COVID-19 patient with dyspnea, increased D-dimer levels, and oxygen saturation < 93. Chest CT evidenced ground-glass opacity with interstitial thickening of the interlobular and intralobular septa, together with pleural effusion (a, b). After contrast media injection, pulmonary embolism was found in the left upper lobar branch, the left inferior lobar branch, and the segmental arteries for the left inferior pulmonary lobe and pulmonary embolism of the interlobar arteries for the inferior right lobe, probably extended to the subsegmentary arteries (c, d).
Pulmonary embolism. COVID-19 patient with dyspnea, increased D-dimer levels, and oxygen saturation < 93. Chest CT evidenced ground-glass opacity with interstitial thickening of the interlobular and intralobular septa, together with pleural effusion (a, b). After contrast media injection, pulmonary embolism was found in the left upper lobar branch, the left inferior lobar branch, and the segmental arteries for the left inferior pulmonary lobe and pulmonary embolism of the interlobar arteries for the inferior right lobe, probably extended to the subsegmentary arteries (c, d)."We're also proceeding with our longitudinal studies in patients with active disease," corresponding author Prof. Marco Francone, PhD, told AuntMinnieEurope.com.
"What is particularly interesting in this setting is the role of cardiac MR with mapping techniques, which is showing ability to unveil clinically silent myocardial damage consisting of tissue edema, necrosis, and fibrosis, through the measurement of T1 and T2 mapping relaxation times," stated Francone, who is past president of the Italian College of Cardiac Radiology and scientific chair of the European Society of Cardiovascular Radiology.
Another important aspect is the prognostic implications of the researchers' collected data, but this is an ongoing project with potential implications for patient management and decision-making (e.g., increased T2 mapping means acute myocardial damage and this potentially yields adverse prognosis).
Overall, this type of research is particularly challenging as it requires meticulous sanitization and safety procedures, to protect patients and exposed personnel, Francone pointed out.



















