A free-breathing, 3D whole-heart T2 MRI mapping sequence can efficiently and reproducibly quantify myocardial T2 times in patients with suspected myocarditis, and potentially even detect more cases of cardiac inflammation than standard 2D T2 maps, according to research published online on 19 January in Radiology.
Researchers led by first author Aurélien Bustin, PhD, and senior author Claudia Prieto, PhD, of King's College London found that their free-breathing 3D T2 mapping sequence was highly reproducible and even enabled confident identification of myocarditis in cases that were inconclusive on T2 mapping.
Further analysis in a larger patient cohort is needed, but "myocardial 3D T2 mapping may be a viable tool for the visualization of inflammation and may potentially afford improved sensitivity," the authors wrote.
Although clinical guidelines recommend the use of established T2 mapping sequences to detect and quantify myocarditis and edema, these sequences are performed in two dimensions with repetitive breath holds and provide only limited coverage of the heart, according to the researchers. In this study, the authors sought to further evaluate an accelerated, high isotropic resolution, free-breathing 3D whole-heart mapping sequence they had previously developed.
The researchers compared the reproducibility of their 3D whole-heart free-breathing technique with 2D breath-hold T2 mapping in phantoms as well as eight healthy participants. They also investigated its clinical performance in 25 patients with suspected myocarditis.
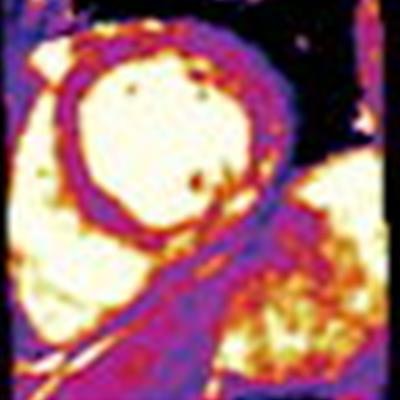
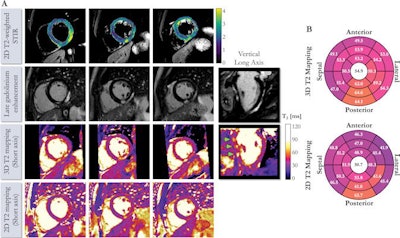 (A) Cardiac MRI scans of a 41-year-old male with suspected cardiac sarcoidosis. Free-breathing 3D whole-heart T2 mapping acquisition time was six minutes and eight seconds. Cardiac cine acquisitions reveal slightly reduced left ventricular ejection fraction (46%). Dense epicardial-to-midwall enhancement of basal to midinferior and lateral walls can be observed, which are typical findings of acute myocarditis. Vertical long axis demonstrates patchy focal midwall regions of enhancement (arrows). (B) 3D and 2D T2 maps. 2D map shows an increase in T2 values (msec) in regions of tissue injury, corresponding to elevation in signal intensity on 2D T2-weighted short inversion time inversion recovery (signal intensity, 2.1). This T2 elevation is less pronounced and appreciable on 2D T2 maps because of partial-volume effects. Image and caption courtesy of Radiology.
(A) Cardiac MRI scans of a 41-year-old male with suspected cardiac sarcoidosis. Free-breathing 3D whole-heart T2 mapping acquisition time was six minutes and eight seconds. Cardiac cine acquisitions reveal slightly reduced left ventricular ejection fraction (46%). Dense epicardial-to-midwall enhancement of basal to midinferior and lateral walls can be observed, which are typical findings of acute myocarditis. Vertical long axis demonstrates patchy focal midwall regions of enhancement (arrows). (B) 3D and 2D T2 maps. 2D map shows an increase in T2 values (msec) in regions of tissue injury, corresponding to elevation in signal intensity on 2D T2-weighted short inversion time inversion recovery (signal intensity, 2.1). This T2 elevation is less pronounced and appreciable on 2D T2 maps because of partial-volume effects. Image and caption courtesy of Radiology.The whole-heart T2 maps were acquired in a mean time of six minutes, 53 seconds at 1.5 mm3 resolution, according to the researchers.
"This approach provides predictable and shorter scanning times that depend only on the participant's heart rate and the number of slices needed to cover the heart," they wrote.
Using the 3D T2 mapping technique, the researchers found that patients with suspected myocarditis had prolonged myocardial T2 values (68 msec ± 7) in comparison with participants without a history of heart disease (51 msec ± 3).
| Reproducibility of T2 mapping MRI in assessing suspected myocarditis | ||
| Breath-hold 2D T2 mapping | Free-breathing 3D T2 mapping | |
| Mean intrasession T2 change | 3.2% | 2.3% |
| Mean intersession T2 change | 4.8% | 4.9% |
After all T2 map datasets were randomly stored, a cardiologist with 11 years of experience then scored map quality using a four-point scoring system and diagnostic confidence on a three-point system. The cardiologist's map quality scores did not differ significantly between the T2 mapping techniques.
In 21 of the 25 patients, interpretations were the same between the two methods. However, in four (16%) cases, cardiac inflammation was found to be present with high confidence on the 3D T2 mapping images but deemed to be inconclusive on the corresponding 2D T2 mapping images.
"Future studies including larger cohorts with myocarditis and myocardial infarction are needed to further establish the clinical use and prognostic value of this noninvasive mapping technique," the authors wrote.
In an accompanying editorial, Dr. Matthias Friedrich of McGill University Hospital Centre in Montreal noted that T2 mapping is complementary with high-sensitivity troponin in identifying the presence -- and cause -- of acute myocardial injury in patients suspected of having acute myocardial disease.
"The unique nature of MRI edema imaging is increasingly well understood in state-of-the-art clinical environments, where myocardial edema imaging is a useful diagnostic tool," Friedrich wrote. "The proposed 3D free-breathing sequence can help simplify this and therefore is a useful step that helps make cardiac MRI in such patients more time and cost-efficient."