Bringing parents into the MRI bore and positioning them head-to-head with their children can help fidgety kids complete cardiac MRI studies without using sedation, according to a report in the November issue of European Journal of Radiology.
"We report a novel approach to scan these patients while they are awake, based on efforts to make them comfortable during the examination as well as distraction from the test itself," wrote Drs. Safwat Aly, a clinical fellow at the University of Toronto in Ontario, Canada, and Lars Grosse-Wortmann, head of pediatric heart care at Oregon Health and Science University in Portland.
Options for keeping toddlers and young children still during cardiac MRI are limited. Due to their inability to cooperate with the procedure without moving around while inside the magnet bore, one of three strategies is usually employed, the authors wrote:
- Accept the risks and potential adverse effects of general anesthesia
- Wait until the patient is older
- Use other imaging modalities, such as CT, which offers limited functional information and entails exposure to ionizing radiation
As an alternative, the authors developed what they called the "parent-child-combination" technique and have used it so far in 16 cardiac MRI scans in 14 patients, 14 of which were successful.
The authors generally consider children between the ages of 3 and 6 for the approach, as long as their caregivers indicate they are likely able to cooperate. The patient is asked to bring a favorite movie to the appointment. On arrival, the procedure is explained in detail to both the parent and the child, supported by a child life specialist as needed.
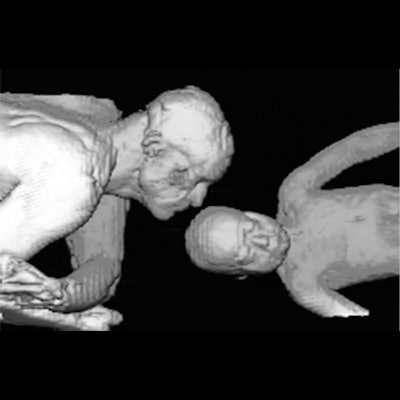
Patients are positioned supine, feet-first into the scanner, with their chest close to the isocenter of the magnet to maximize the MR signal from the receiver coils. The parent is positioned in the decubitus position facing their child, head-first into the scanner, as close to the child as possible without being in the field of view. This soothes the patient without sacrificing scan time, the authors wrote.
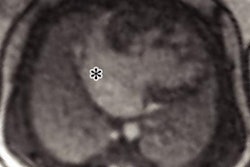
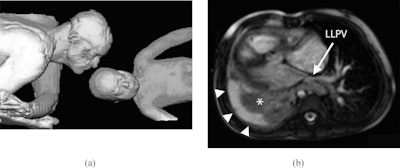 (A) Volume-rendering reconstruction of father and daughter in MRI scanner bore. (B) Axial image from a steady-state free precession acquisition. LLPV = left lower pulmonary vein.
(A) Volume-rendering reconstruction of father and daughter in MRI scanner bore. (B) Axial image from a steady-state free precession acquisition. LLPV = left lower pulmonary vein.In one case highlighted in the series, the authors used the technique in a 2.5-year-old girl born with several heart defects. The girl had undergone biventricular repair and developed right lower and middle pulmonary vein stenosis and presented with recurrent pneumonia and chronic right pleural effusion.
The girl underwent cardiac MRI together with her father. All images were acquired during free breathing, and pauses in scanning were minimized to shorten scan time and allow the patient to focus her attention away from the test itself, the authors explained.
The examination revealed mild narrowing of the patient's left lower pulmonary vein and of the distal right ventricle to pulmonary artery conduit. Both ventricles were dilated with reduced ejection fractions. There was collapse/consolidation of the patient's right lung and a large right pleural effusion.
The girl subsequently underwent percutaneous pulmonary valve implantation, the authors wrote.
The parent-child-combined technique is more time-consuming, but the draw on resources is likely less than when examining these patients under general anesthesia or sedation, the authors noted. Moreover, evidence suggests an increased risk of adverse neurodevelopmental outcomes in children exposed to general anesthesia at a young age, they added.
"This workflow is applicable not only to [cardiac MRI], but other indications for magnetic resonance imaging as well," the authors concluded.