High-dose-rate (HDR) brachytherapy is increasingly employed to treat localized prostate cancer, with MRI guidance used to ensure precise localization of the tumor and surrounding tissues. Researchers from University Medical Center Utrecht (UMCU) in the Netherlands have now devised a way to optimize the dose delivery further.
HDR brachytherapy involves inserting needles or catheters into the tumor and stepping a radioactive source through according to a calculated dose plan. Unexpected events, however, such as suboptimal needle positioning or internal organ motion can still lead to incomplete target coverage or overdose of organs-at-risk.
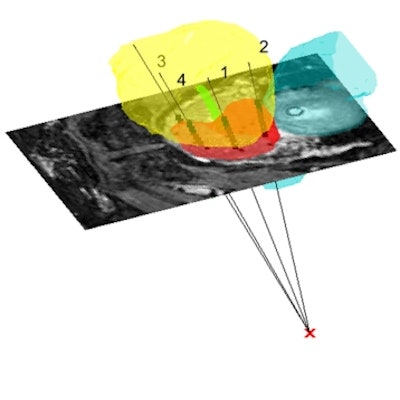
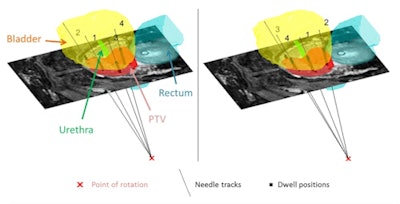 Final needle trajectories and dwell positions for a typical patient resulting from one simulation in the situation of optimal (a) and least optimal (b) needle insertion sequence. The order of needle insertion is depicted at the tip of the needle.
Final needle trajectories and dwell positions for a typical patient resulting from one simulation in the situation of optimal (a) and least optimal (b) needle insertion sequence. The order of needle insertion is depicted at the tip of the needle.To improve treatment accuracy, the researchers developed a pipeline in which the dose plan is updated using feedback on needle positioning errors. However, the needle insertion sequence is chosen by the doctor and may potentially be suboptimal. In their latest work, they present an automatic needle sequencing strategy for MR-guided HDR prostate brachytherapy. They assessed their proposed sequencing strategy using simulations of HDR prostate brachytherapy on 11 patients (Physics in Medicine and Biology, 20 April 2017, Vol. 62:10, pp. 4031-4035).
"Our motivation was to provide a tool to assist the doctor in determining the optimal needle insertion sequence," explained first author Maxence Borot de Battisti, who is a doctoral student. "Moreover, it is a step toward the development of a fully automatic control system, where the dose plan and needle insertion sequence are automatically reoptimized during the intervention."
Testing plan quality
The sequencing strategy involves inserting each needle into the most sensitive (in terms of the effect of positioning errors on dose distribution) needle track. To predict track sensitivities, the researchers developed a stochastic method based on needle insertion simulations. During treatment, the needle position is measured and the dose plan updated accordingly. Following dose delivery, track sensitivities are recalculated to determine the next track to use. In this way, any errors resulting from the first needle insertion can be determined and compensated for in subsequent insertions.
 Maxence Borot de Battisti from University Medical Center Utrecht.
Maxence Borot de Battisti from University Medical Center Utrecht.A dose plan for prostate HDR brachytherapy is considered clinically acceptable when doses to the planning target volume (PTV) and OARs (urethra, rectum, and bladder) meet a specified set of constraints. At the UMCU, these constraints are: 19 Gy or more to 95% of the PTV (D95% PTV); below 21 Gy to 10% of the urethra (D10% Ur); and less than 12 Gy to 1 cc of rectum (D1cc Rec) and to 1 cc of bladder (D1cc Bl).
To test their proposed needle sequencing strategy, Borot de Battisti and colleagues simulated HDR prostate brachytherapy procedures on 11 patients with 4, 6, 8, 10, and 12 needle insertions (55 scenarios). For each insertion, they simulated optimal needle positioning, as calculated from the initial dose plan, and simulated suboptimal needle positioning by adding a random angulation error. All simulations were repeated 100 times. They compared cases in which the least sensitive needle track was selected for insertion ("least optimal" sequence) with corresponding cases where the most sensitive needle track was selected ("optimal" sequence).
For a typical patient with four needle insertions, the final dose parameters with optimal needle positioning were 20.0, 19.8, 8.6, and 10.9 Gy, for D95% PTV, D10% Ur, D1cc Rec, and D1cc Bl, respectively. With suboptimal needle positioning, median doses were 19.2, 20.5, 8.2, and 11.2 Gy for the least optimal needle sequencing scenario, and 19.4, 20.3, 7.9, and 10.7 Gy using the proposed optimal needle sequencing.
The researchers also assessed plan quality for different numbers of needle insertions, using the evaluation parameter, E, which represents the minimum difference between a dose coverage parameters and a constraint. A higher value of E represents a better quality plan. For one example patient, with 4, 6, 8, 10, and 12 needle insertions, the median value of E was 0.2, 0.8, 1.5, 1.7, and 1.8 with least optimal sequencing, and 0.4, 1.3, 1.6, 1.8, and 2.0 with optimal sequencing. In several cases, optimal sequencing had a greater effect on dose coverage for a small number of needle insertions -- implying that this approach may be more important for treatments using fewer needle insertions.
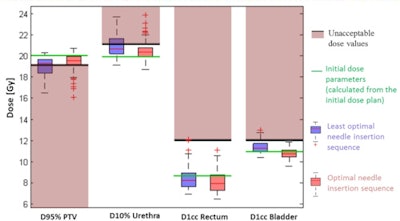 Final dose parameters resulting from the 100 simulations for optimal and least optimal needle insertion sequences. The green and black lines represent the preplan dose parameters and the clinical constraints, respectively.
Final dose parameters resulting from the 100 simulations for optimal and least optimal needle insertion sequences. The green and black lines represent the preplan dose parameters and the clinical constraints, respectively.Overall, simulations showed the optimal needle sequence improved dose distributions in 91% of scenarios tested, with increased PTV dose and decreased dose to OARs. The computation time for sequencing was less than 6 seconds per needle track (using MatLab 2015), suggesting that this tool could be used during a brachytherapy procedure.
"Our goal is to clinically implement MR-guided HDR prostate brachytherapy using a single needle robotic device to support needle insertions. The clinical workflow will integrate the proposed sequencing strategy," Borot de Battisti said.
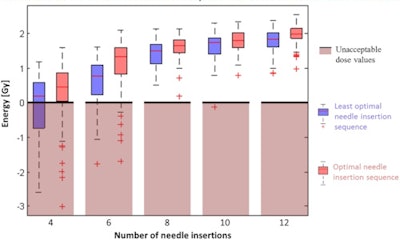 Dose plan quality as a function of the number of needle insertions and the needle insertion sequence.
Dose plan quality as a function of the number of needle insertions and the needle insertion sequence.The researchers are currently working on several projects to enable clinical implementation of this approach. This includes developing a tool for deformable registration of diagnostic and intraoperative MR-images, a protocol for inserting a brachytherapy needle under MR-guidance and a single-needle robotic device for MR-guided needle insertion.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.