What is the best way to maximize tumor control? Should we "crank up the volume" or "turn off the switches"? That was the intriguing theme of a debate at the recent European Society for Radiotherapy and Oncology (ESTRO) 35 conference in Turin, Italy. Pitting physicists against biologists, the ensuing discussion examined whether physics- or biology-based developments will better progress radiation therapies.
At the start of the debate, a show-of-hands vote revealed an audience preference for a biological approach. Could the speakers change the attendees' minds?
Reimagine the future
First to the podium, Bradly Wouters from the Princess Margaret Cancer Center argued the case for "turning off the switches" and exploiting knowledge of cell signaling, genetics, and cell biology. He described three aspirations in radiation oncology-driven cancer treatment, the first being improvement of local tumor control. He pointed out the progression of radiotherapy from 3D conformal to intensity-modulated, image-guided and adaptive treatments has certainly improved outcomes for patients, but that ongoing technical developments are now producing smaller gains.
 Alison Tree, from the Institute of Cancer Research and the Royal Marsden, and Bradly Wouters from the Princess Margaret Cancer Center presented the case for "turning off the switches."
Alison Tree, from the Institute of Cancer Research and the Royal Marsden, and Bradly Wouters from the Princess Margaret Cancer Center presented the case for "turning off the switches."While radiation is highly effective, the same can be said for cancer drugs, Wouters noted, citing the success of drugs developed to treat melanoma with the V600E BRaf mutation. "But even 'near perfect' drugs are limited by biology," he explained. When melanoma patients relapse after therapy, a physicist would say "give more drug, more conformal drug" -- but the problem is not the drug's not effective; the problem is the biological diversity in tumors. The way to achieve significant gain, Wouters proposed, lies in targeting that diversity, using knowledge gained from biopsies and imaging to tailor individual therapies and increase cure rates.
A second aspiration is treatment of systemic disease including oligometastases. The problem here, Wouters said, is "you can only treat what you can see -- and patients inevitably have cells that you can't see." Biological approaches such as immunotherapies may come into play here.
The third aspiration is reducing toxicity in cured patients. While normal tissue exposure will inevitably always be part of curative radiotherapy, there are new biological ways to approach this problem, via protection or regeneration of tissue. So why has biology not had a big impact in the field yet? "We're in the middle now, aiming for transformative change," Wouters said. "The question is, do we want more of the same, or to reimagine the future?"
Technology is key
"The past, the present, and the future of radiation oncology is dominated by technological innovations," declared Jan-Jakob Sonke from the Netherlands Cancer Institute. Stating the case for keeping the focus on physics, Sonke noted that where we are now in the clinic is mostly due to physics, following a century's worth of innovation; the only biology involved is fractionation.
 Jan-Jakob Sonke from the Netherlands Cancer Institute and Andre Dekker from MAASTRO argued the case for physics.
Jan-Jakob Sonke from the Netherlands Cancer Institute and Andre Dekker from MAASTRO argued the case for physics.One area ripe for improvement is global radiotherapy resources. Sonke pointed out only 40% of patients worldwide currently have access to radiotherapy. The cost to increase global access to state-of-the-art radiotherapy is estimated at $184 billion U.S. (163 billion euros), but would provide a saving of some 26.9 million life-years and a net monetary benefit of $278 billion U.S. (246 billion euros). Such an undertaking would capitalize on existing technology innovations. It would require training of physicians and physicists but, Sonke noted, no radiation biologists would be required.
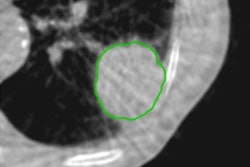
Sonke argued that upcoming technological innovations will further widen the therapeutic window. Adaptive replanning, for example, enables increased tumor dose by accounting for inter- and intrafractional changes. Another recent advance is the introduction of dose painting. "It took a while to bring this to the clinic, but now trials are ongoing," he said. "We can deliver higher doses to regions of tumor, without extra organ-at-risk exposure."
Other developments include the proliferation of proton therapy, as well as the increasing use of carbon ion beams where, Sonke said, it is possible to exploit biology without using radiation biologists. Improvements in imaging systems will reduce the detectable lesion size, while the introduction of MR-guided radiotherapy will shrink treatment margins and lower toxicity.
Finally, Sonke highlighted the emergence of machine learning applications within medicine, with neural networks enabling analysis of large amounts of data, and radiomics furthering the understanding of tumor and normal tissue toxicity. Deep learning technology could identify the most radiosensitive patients and personalize their treatment accordingly. "There is some place for biology," Sonke concluded. "But not much."
Drug addition
Back to the biology, Alison Tree from the Institute of Cancer Research and the Royal Marsden took a look at the possibilities offered by adding drugs to radiation treatments. "Radiation has helped cure many cancers," she said. "However, its use in isolation has limitations that cannot be overcome by simple dose escalation."
For example, glioblastoma patients treated with dose-escalated radiotherapy exhibited a median overall survival of just 20 months. Patient data revealed that the tumor grows even in high-dose areas -- it is simply not possible to deliver enough dose to achieve local control. Tree described a decade of studies examining the long-term impact of approaches including dose escalation, nodal irradiation, image-guidance, and simultaneous integrated boost for treating prostate cancer. "As far as we can tell, not one of these made a single patient live a day longer," she stated.
Instead, drugs are needed that can shift the therapeutic curve to the left, and increase cure with less toxicity. Tree cited a recent paper on the integration of chemoradiation with molecularly targeted therapy. The authors proposed that exploiting biological differences between cancer and normal tissue might increase efficacy while maintaining tolerable toxicity. Promising approaches include combining chemoradiation with agents that modulate tumor-specific pathways, target the immune system, or target angiogenesis.
This is not a new idea, Tree said, describing a study published in 2001 in which prostate cancer patients received radiotherapy with or without androgen suppression. Adding androgen suppression improved the 10-year overall survival from 40% to 58%. "When did you see improvements like that in radiotherapy?" she asked. Promising results have also been reported for combining immunotherapy (for example, drugs that turn off the T cell inhibitor PD-L1) with radiation.
"We have already 'cranked up the volume,' and spent half a century perfecting our techniques," Tree concluded. "But if you only have a hammer, you see all problems as a nail -- we now need to break out the power tools and benefit patients."
Too complex a system
The last speaker, Andre Dekker from MAASTRO, aimed to persuade the audience that "we need less biology." Tumors and normal tissues are complex systems, he explained, and we don't yet understand complex systems. As such, it is extremely hard and sometimes impossible to predict what will happen. Instead, suggested Dekker, we need to stick to the basic science. "It is too early to start switching, you'll break things," he said.
Dekker took a look at the current success of drug development in biology, noting that only 15% of drugs make it from phase I trials to clinical approval. And in oncology, only 7% of drugs are approved, because of efficacy and safety issues. He also emphasized the inconsistency associated with biology. For example, only six of 53 "landmark" cancer studies by the biopharmaceutical company AMGen were reproduced, while published target-validation results from pharmaceutical company Bayer were reproduced in only 14 of 67 of projects.
Dekker cited a 2015 study that estimated the cost of irreproducible biology research at $28 billion (25 billion euros) per year in the U.S. "And even if you get a drug that works, it's going to cost you," he added, quoting the price for one year of life at $207,000 U.S. (183,000 euros) in 2013. "As Jan-Jakob said, physics just needs $184 billion (163 billion euros) to save 27 million life-years, that's $7,000 (6,000 euros) per life-year, two orders of magnitude cheaper than biology."
End game
The debate was rounded off with challenges posed from the biologists to the physicists and vice versa. The physicists were asked whether they have now reached the pinnacle of their field, with no way to substantially improve outcomes. Sonke disagreed, citing fractionation, machine learning, and individualization of treatment as ways forward. "And our toolset is sufficient to achieve this," Dekker added.
 A show-of-hands vote at the end of the debate said the majority of the audience pick biology as the way forward.
A show-of-hands vote at the end of the debate said the majority of the audience pick biology as the way forward.Dekker then challenged the biologists to convince him that in the next five to 10 years biology will be quantitative not qualitative, and move toward having effects in the full population. "We don't need to fully understand biological systems to intervene and have an effect," Wouters replied, citing the example of the breast cancer drug Herceptin. "You don't have to understand everything about it to make patients' lives better," Tree concurred.
The session finished with a second show-of-hands vote. Again, the majority of the audience picked biology as the way forward, but the result was a close call, with an increased number thinking physics to be a better option. As such, the session chairs declared both sides to be winners.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.