Ultimately, MRI guidance could be applied to improve all radiotherapy techniques, including proton therapy. Last month, Bas Raaymakers, PhD, from Utrecht University in the Netherlands took a glimpse into the future and explained why clinical implementation will require large-scale collaborations.
 Bas Raaymakers presents his inaugural lecture. Image courtesy of Roy Sanders.
Bas Raaymakers presents his inaugural lecture. Image courtesy of Roy Sanders.Whilst working at UMC Utrecht, Raaymakers has played a central role in the creation of the MRI-linac, a 1.5-tesla MRI-guided radiotherapy system. Addressing an audience of colleagues, family and friends -- as well as 100 or so attendees of the symposium "From vision to sight: The MRI Linac," organized to precede the inaugural lecture -- Raaymakers discussed what the future may hold for this potentially transformative technology.
In the majestic setting of Utrecht University's Academiegebouw, Raaymakers began by explaining why he and his colleagues started to develop a new treatment system, back in 1999. "To quote Professor Oelfke from the Institute of Cancer Research in London: 'In radiotherapy, we are trying to hit an invisible target with an invisible beam,' " he said. And as radiation therapy is usually fractionated, anatomy and tumor variations can occur between, as well as during, fractions. "Right now, all of this is invisible to us during radiation delivery," he added.
The conventional way to deal with anatomical changes is to include margins that guarantee tumor coverage, but this comes at the price of irradiating normal healthy tissue. As such, much research effort is being put into estimating tumor location during radiation delivery. Cone-beam CT can be employed to visualize lung tumors, for example, while fiducial markers are used in prostate treatments.
"But we want this high-precision, highly effective radiotherapy for any tumor," Raaymakers said. "We don't want to estimate the tumor position; we want to see it during radiation delivery. MRI can offer this."
Herein lies the motivation for the MRI-linac. "We want to bring sight to radiation oncology and offer the ability to change the treatment based on what we see," Raaymakers said. "I think that in the future, radiation oncologists will shiver when they think back to the time when you couldn't see what you were doing during delivery."
 Bas Raaymakers and the Utrecht University professors prepare for the inauguration ceremony. Image courtesy of Roy Sanders.
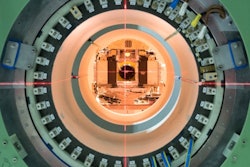
Bas Raaymakers and the Utrecht University professors prepare for the inauguration ceremony. Image courtesy of Roy Sanders.In collaboration with Elekta and Philips Healthcare, the UMC Utrecht team developed the MRI-linac. The first prototype, built in 2009, showed that diagnostic quality 1.5-tesla MR images could be achieved in the presence of a radiation beam (see: MR-guided radiotherapy: proof of concept). The second version, which added a rotating gantry and multileaf collimator, demonstrated intensity-modulated radiotherapy and beam gating and tracking.
The latest version is a clinical prototype, being commercialized by Elekta and introduced via a consortium named Atlantic, and currently shipping to research facilities (see: Commercializing MRI-guided radiotherapy). Elekta plans to start selling the MRI-linac in 2017, with the first units shipped the following year. Raaymakers suggests that given the growing interest in MRI-guided radiotherapy, "growth will be limited by production capacity, not customers."
What's needed next?
Raaymakers described some of the specific technical requirements for bringing MRI into radiotherapy. The MR system needs to provide fast 4D imaging for tracking geometrical changes during treatment. Modeling and motion prediction are also important, as is the ability to calculate dose distributions and evaluate treatment response using the MRI data. He noted that such tasks will create a new research arena for MRI physicists working within radiotherapy departments.
 Bas Raaymakers in front of Elekta's Atlantic system with Robert Spaninks, Elekta service engineer. Image credit: PRNewsFoto/Elekta.
Bas Raaymakers in front of Elekta's Atlantic system with Robert Spaninks, Elekta service engineer. Image credit: PRNewsFoto/Elekta.Effective image processing tools are also required to interpret the MR data. Currently, physicians delineate structures manually, but for the MRI-linac, real-time automated delineation becomes a necessity. Likewise, there's a need for real-time plan adaptation. "Once we have a continuously updated patient anatomy, we then have the responsibility to do something with this information," Raaymakers explained. "We should adapt the dose distribution to the latest anatomy. And the more frequent the adaptations are, the higher the need for automatic treatment planning."
Finally, for safe clinical implementation of the MRI-linac, new quality assurance (QA) procedures must be developed. Delivering radiation within a magnetic field opens up a new set of QA requirements, because both the dose distribution and the radiation detectors themselves will be affected by the field. Raaymakers and colleagues are currently evaluating such QA detectors and phantoms from a range of vendors. Meanwhile, the U.K.'s National Physical Laboratory (NPL) and VSL, the National Metrology Institute of the Netherlands, are creating new dosimetry standards for magnetic fields.
Clinical translation
"MRI-linac technology is here, or close to here," Raaymakers said. "So now what?" He predicts that the MRI-linac will have a substantial impact on clinical treatments -- being far more than just another new radiotherapy machine. The overall aim is simple: radiotherapy with more cure and less toxicity for all tumor sites, including those that can't be treated with existing equipment.

"When radiation oncologists can see what's being hit by beam, radiotherapy becomes like a surgical procedure, but without the knife," he explained. For example, it may be possible to replace invasive partial nephrectomy used to treat kidney cancer with ablative radiotherapy delivered as an outpatient procedure.
Raaymakers noted that clinical implementation will require large-scale collaborations, such as Elekta's Atlantic research consortium. In addition, other research groups worldwide have adopted the idea of MRI-guided radiotherapy. Paul Keall and his group at the University of Sydney are building a hybrid 1-tesla MRI linac, Gino Fallone and colleagues at the Cross Cancer Institute in Edmonton have an operational prototype 0.5-tesla machine, while ViewRay's 0.3-tesla MRI cobalt radiotherapy systems are already treating patients.
"We would have liked to have been the first to treat patients, but it is good to see the idea being picked up," Raaymakers said. "We should all team up to convince the community of the added value of MRI-guided radiotherapy."
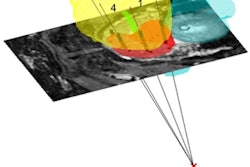
 Proton therapy plans for liver (top row) and larynx (bottom row) treatments, generated without (left) and with (center) a 1.5-tesla field; the dose difference is shown on the right.(from Phys. Med. Biol. Vol. 60:15, pp. 5955).
Proton therapy plans for liver (top row) and larynx (bottom row) treatments, generated without (left) and with (center) a 1.5-tesla field; the dose difference is shown on the right.(from Phys. Med. Biol. Vol. 60:15, pp. 5955).The time has now arrived for the start of clinical trials on the MRI-linac. The researchers have drawn up a shortlist of anatomical sites and "safe and simple" trials will soon begin. The "first-in-man" treatments will be of spinal bone metastases, with the aim of demonstrating the technological feasibility and safety of the system. On-board portal imaging will enable independent verification of the MRI localization.
"All of the technology has to come together to prove that the MRI-linac can be brought safely into the clinic," Raaymakers said. "After this, the real exciting times will start. Different tumor sites will be used to demonstrate the clinical benefit of MRI-guided radiotherapy. I am convinced that the results will, in the end, be something to celebrate together."
Future gazing
Ultimately, MRI guidance could be applied to improve all radiotherapy techniques, including proton therapy. "Often, the MRI-linac and proton therapy are seen as being in opposition," Raaymakers explained. "But both are trying to achieve the same goal -- more accurate dose delivery with less toxicity." MR imaging closes in on this goal by providing sight, while proton therapy achieves it by stopping the dose at the appropriate location in the patient.
"We should go for a hybrid system," Raaymakers said. "It's simply too cool not to do it." As such, the Utrecht team are working to quantify how the two technologies interact, to provide the rationale for developing a prototype. "I am convinced that MRI-guided proton therapy could be the next great step forward," he said.
MRI is also used for guidance of other clinical modalities, such as brachytherapy, where it already provides a clinical standard for treating cervical cancer. Utrecht researchers are also working to optimize MRI-guided high-energy focused ultrasound (HIFU). "We should optimize all of these modalities individually, but at the same time, optimize a multimodal treatment," Raaymakers suggested.
Raaymakers concluded his inaugural lecture with some comments on UMC Utrecht's Center for Image Sciences. He pointed out that the center includes researchers with expertise in the whole spectrum of specialties required to progress a project like the MRI-linac. These researchers now plan to investigate the various techniques, including multimodality approaches, and compare clinical results and cost-effectiveness.
Taking things a step further, the MRI-linac may one day deliver one-stop-shop procedures with diagnosis and treatment performed using the same machine. "This is the best place on Earth to develop technologies and transfer them into the clinic," Raaymakers said.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.