
Online MRI-guided radiotherapy enables real-time, high-precision visualization of anatomical changes during treatment delivery. But with many image-guided radiotherapy (IGRT) options available already, how great is the need for large-scale in-room MR guidance? This was the question under debate at the recent European Society for Radiotherapy and Oncology (ESTRO) 35 conference in Turin, Italy.
"Do we want a system that allows us to see what we are treating in real time? Yes absolutely," said Dr. Frank Lohr from the University Medical Center Mannheim. "But the economics have to be justified." Lohr questioned whether online MRI guidance will really make a qualitative difference, or whether we should instead focus on exploiting the advanced image-guidance strategies that are already available. He indicated that online MRI guidance may have implications in two areas: geometrical treatment accuracy and biologically/functionally driven strategies.
 Frank Lohr from the University Medical Center Mannheim presenting at the ESTRO 35 conference.
Frank Lohr from the University Medical Center Mannheim presenting at the ESTRO 35 conference.Lohr first considered the current accuracy status in radiotherapy. The main problem is breathing motion, which can create uncertainties in dose delivery and target coverage. Margins are applied to account for such motion, but at the expense of normal tissue irradiation; while approaches such as breath-hold, gating, and tracking enable margin reduction.
As for where the improved geometric accuracy may create a better outcome, Lohr said it could benefit large lung and liver tumors, and possibly targets in the kidney and pancreas. For small lung and liver targets, it is unlikely that better geometric accuracy will further improve results. He also noted that current MRI-guided radiotherapy systems cannot deliver noncoplanar beams.
"We already have tools that get us to near perfect accuracy," Lohr said, citing the Gamma Knife and CyberKnife radiosurgery systems, and motion-tracking systems such as ExacTrac and Calypso. "And brachytherapy already uses MRI guidance."
So what level of accuracy can be achieved with guidance approaches available on conventional linacs today? Cone-beam CT (CBCT) with deep inspiration breath-hold (DIBH) can achieve an accuracy of 2-3 mm, Lohr said, noting that DIBH used to be cumbersome and slow, but is now faster and easier to perform. This approach was facilitated by the development of flattening filter-free delivery and fast collimators that shorten the treatment duration, as well as positioning devices such as surface scanners and fiducial tracking. In addition, recent work in applied physiology has indicated that breath-holds of several minutes can be sustained with minimal preparation.
Another technology that may return to mainstream use is ultrasound, which offers excellent soft-tissue image quality where applicable and benefits from improved tracking algorithms.
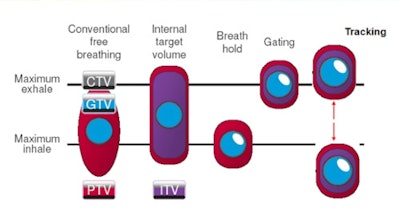 Breathing motion can be addressed using approaches such as margins, breath-hold, gating, and tracking.
Breathing motion can be addressed using approaches such as margins, breath-hold, gating, and tracking.Finally, Lohr considered MRI's unique ability to image physiological variations. The ability to identify functionally active lung tissue and optimize radiation delivery to avoid these areas, for example, could prove of massive benefit. "But how much of this information is needed on a minute-by-minute basis?" he asked. "Could this be performed offline?" He noted that online MR-based functional imaging is limited by currently available field strengths. Should this change, however, and targets identified that require high-resolution dose deposition and daily changes in targeting strategy, this could represent the ultimate application of online MRI guidance.
Lohr reiterated the precision treatment delivery afforded by today's IGRT approaches. "If we really need online MR guidance, shouldn't we do everything we can with what we already have to get as near as possible?" he concluded.
Making the case for MRI
"The organizers gave me the easiest job in the world," declared the University of Sydney's Paul Keall, PhD, "To convince you that the future of radiotherapy involves integrated MR-guided machines." Keall went on to list 10 reasons why the unparalleled soft-tissue contrast afforded by MRI is essential.
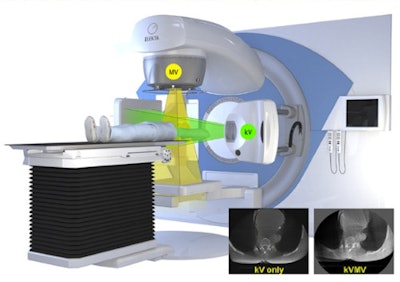 Deep inspiration breath-hold with ultrafast kVMV cone-beam CT guidance.
Deep inspiration breath-hold with ultrafast kVMV cone-beam CT guidance."It's obvious," he said. "We need to see the tumor anatomy throughout treatment." He asked the audience to close their eyes and then shake hands with the person next to them. "This is what we're doing now in radiotherapy."
Keall emphasized that patient motion is complex, with translations, rotations, deformations, and changes in physical properties to account for. "Our patients are dynamic, our anatomy is dynamic, and our physiology is dynamic," he said. And it's not just target motion that needs tracking. If a tumor is located next to the heart, for example, MRI can visualize the beating heart to reduce treatment toxicity. And while ultrasound imaging may be cheaper, image quality is far superior with MRI and of particular benefit in sites such as the kidney and liver.
Looking at the introduction of other advanced radiotherapy technologies, a show-of-hands revealed that almost all of the audience now performs stereotactic body radiotherapy, whereas 10 years ago only about 20% were using this approach. Likewise, almost everyone now employs some form of image guidance, while less than 10% were doing this 10 years previous. "I think that what we're doing with MRI is the same," Keall said.
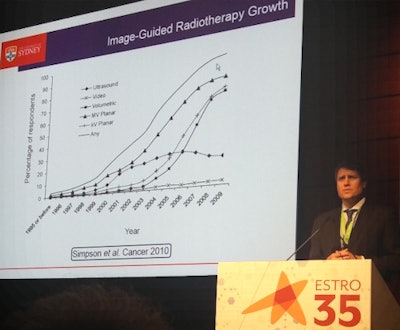 Paul Keall from the University of Sydney.
Paul Keall from the University of Sydney.He listed the many companies and institutions now building MR-guided radiotherapy devices. This includes ViewRay, with 20 confirmed sales to date and Elekta, which plans to ship 79 units by 2019 -- a combined market of $1 billion U.S. (884 million euros). Last year, the University of Alberta group founded Magnet-Tx to commercialize its Aurora RT, while both Siemens and the Australian MR-linac program demonstrated prototypes.
Other reasons for implementing online MR guidance include the ability to exploit existing MRI expertise, the lack of imaging dose, and the ability to image actual anatomy as opposed to surrogates.
MR guidance could also enable radiation treatment of nononcologic diseases such as atrial fibrillation, currently treated via an invasive, expensive procedure. By using MRI to image the beating heart and define the small, moving target volumes, it's possible to noninvasively treat one of the most common conditions. And if physicians start to use radiation for this application, more radiotherapy departments will be needed.
Finally, Keall described the use of online MRI guidance to enable physiological targeting during radiotherapy, which no other technology can achieve. "Cancer physiology is heterogeneous and changes with time," he said, citing tumor hypoxia, which can change during a single treatment. "The ability to selectively image and target the most resistant parts of cancer could dramatically change cancer outcomes."
Are we already good enough?
Retaking the stage, Lohr addressed some of Keall's arguments. Yes, MR guidance is obvious, he agreed, but only if you've got the money. With MR-guided systems costing three times that of other radiotherapy devices, the question is "How much good can we achieve with more imaging?" Lohr also noted many professionals still do not concur that daily online imaging is useful.
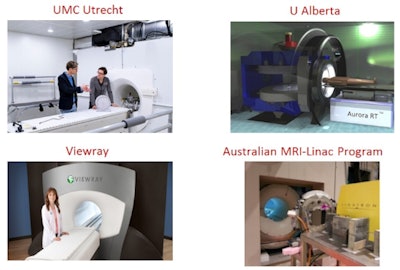 MR-guided radiotherapy devices are being built by groups including Elekta (in partnership with the University of Utrecht and others), the University of Alberta, ViewRay, and the Australian MR-linac program.
MR-guided radiotherapy devices are being built by groups including Elekta (in partnership with the University of Utrecht and others), the University of Alberta, ViewRay, and the Australian MR-linac program.Direct imaging of the tumor is already possible, Lohr said, if you treat in a static breath-hold situation, which can be created today. He noted that using MRI to enable radiation treatments of atrial fibrillation is indeed promising and merits evaluation.
As for functional imaging, Lohr again questioned whether currently available field strengths are sufficient and wondered which processes change within minutes and thus necessitate online imaging. Functional information could instead be gathered offline, he suggested, and integrated into treatment plans. "We shouldn't feel too bad, because we're already pretty good at what we're doing," he concluded.
Finally, Keall countered some of Lohr's concerns. In terms of whether improved geometric accuracy leads to a better outcome, he emphasized that motion is the biggest error in the radiotherapy dosimetry chain. As for the inability of current MRI-guided radiotherapy systems to use noncoplanar beams, Keall explained that coplanar beams are most common in today's treatments. "If it turns out that multiple coplanar beams are used more in the future, we can work to integrate MR machines to do this," he said.
As for the system cost, Keall noted when integrated PET/CT systems were first introduced, people questioned the need to merge two expensive machines. But the benefit of integration was strong enough to justify itself, and all PET systems are now integrated with CT. "It is cost-effective to add image-guidance to reduce toxicity," Keall concluded.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.



















