
The excessive use of abdominal radiography (AXR) in the emergency department adds financial strain, increases patient discomfort, and may even be a source of future litigation, U.K. researchers have found.
"Should AXRs be superseded by more definitive imaging modalities in emergency medicine for acute abdominal pain?" asked Dr. William Maynard, from the University of Birmingham, Heart of England National Health Service (NHS) Foundation Trust (HEFT) at last month's U.K. Radiological Congress (UKRC). "This may reduce inappropriate requests and needless radiation."
Abdominal radiographs rarely aid future patient management and are known to have limited diagnostic value in the acute setting, with only 19% showing abnormalities in a Canadian study (Kellow et al, Radiology, Vol. 248:3, pp. 887-893), according to Maynard and colleagues.
Poor compliance to U.K. Royal College of Radiologists (RCR) guidelines on the use of AXRs in emergency care has been demonstrated in many studies, and the rates of adherence range from 32% to 43%, they explained in an e-poster. These examinations deliver a radiation dose 30 times that of a chest radiograph, according to the iRefer guidelines tool from the RCR, and overuse leads to unnecessary radiation exposure and increased costs.
"AXRs are routine in acute abdominal management, despite their limited diagnostic value," they noted. "The low diagnostic value can be partly explained by the poor clinical adherence to the reference criteria and subsequent inappropriate investigations. This is hidden by misleading information given on referral forms, the reasons for which could be pressure from senior clinicians, defensive practice, poor knowledge of the amount of radiation exposure from an AXR, and inaccurate note taking."
Gathering the data
In their study presented at UKRC 2015, Maynard et al aimed to evaluate the number of requests for abdominal radiography studies that adhered to HEFT's guidelines from the accident and emergency department (A&E); to establish whether there is concordance between the AXR request forms and the clinical history in the A&E primary assessment document; to ascertain the number of positive and negative findings according to the radiologist's report; and to determine the number of patients receiving further imaging in the same admission as well as of the modalities they received.
The researchers conducted a retrospective analysis of 198 adult patients attending A&E at Good Hope Hospital in Birmingham over a four-month period. Patient number, age, date of study, primary reason for request on referral form, clinical reason for request, AXR findings, further imaging, and reason for further imaging were collected each patient.
The data were collected by means of patient case notes using the electronic patient record (iCare Vortal), electronic radiology request cards, and radiological findings. To allow quantitative analysis, the data were organized and codified.
Around 30.3% of abdominal radiographs had positive findings. About 38% of patients received further imaging during the same admission, with 27% having a CT scan.
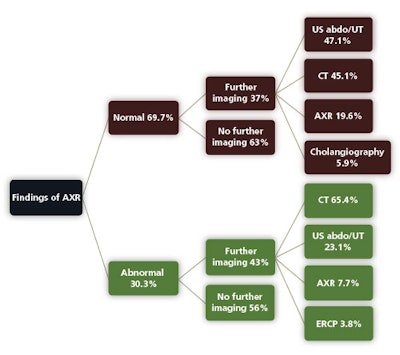 Outcome of a study involving 198 adults who underwent emergency abdominal x-ray at Good Hope Hospital over four months. UT = uterus, ERCP = endoscopic retrograde cholangiopancreatography.
Outcome of a study involving 198 adults who underwent emergency abdominal x-ray at Good Hope Hospital over four months. UT = uterus, ERCP = endoscopic retrograde cholangiopancreatography.Overall, Maynard and colleagues recommend providing more education about the necessity of a detailed, accurate, clinical history on the relevant form to emergency clinicians, and limiting futile abdominal radiographs from the radiologists' perspective. Also, to rectify the lack of knowledge of AXR guidelines, they advocate raising awareness of local and national guidelines and the dose burden of AXRs. This proved a success in a previous study at the University Hospital of Wales in Cardiff, U.K., where inappropriate referrals were cut from 30% to 7% (Annals of the Royal College of Surgeons of England, May 2006, Vol. 88:3, pp. 270-274).
Finally, highlighting the introduction of the RCR phone application, iRefer, to clinicians would allow increased accessibility to guidelines in a fast-paced environment, they concluded.



















