
I was very interested to read your article about the recent audit on the inappropriate use of abdominal radiographs at the Sandwell & West Birmingham Hospitals National Health Service (NHS) Trust in the U.K., and I wanted to share my own experiences.
In July 2016, I conducted a similar audit over a one-month period in a major teaching hospital in the Republic of Ireland where 187 plain-film abdominal x-rays were reviewed using the U.K. Royal College of Radiologists' (RCR) guidelines. These did not include outpatient requests as in the Sandwell & West Birmingham audit, but rather requests for plain-film abdominal x-rays in a busy emergency department that dealt with the adult and pediatric population.
The requests were reviewed to see whether: 1) a clear question was asked of the interpreting radiologist 2) was the radiograph request indicated in keeping with RCR guidelines 3) was there a significant abdominal pathology identified?
Firstly, 52% (97/187) of requests did not ask a clear question of the interpreting radiologist, nor could a clinical question be reasonably inferred from the requesting text. Based on the clinical information given in the requesting text box, the x-rays were deemed to be clinically indicated in only 71 cases (71/187; 38%), however in a third of cases (57/187; 30%) there was insufficient clinical information given to assess whether or not the scan was indeed indicated. The remaining third of scans performed (59/187; 32%) were not clinically indicated.
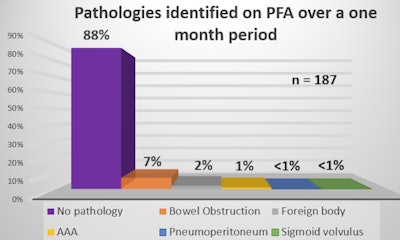 Pathologies identified on plain-film abdominal x-ray (PFA) over a one-month period.
Pathologies identified on plain-film abdominal x-ray (PFA) over a one-month period.One of the radiology reports in this group went so far as to say: "Please note that the clinical history given is not an indication for exposing a child to radiation." Another report outlined that this was the third time the patient was exposed to an abdominal x-ray when the previous radiology reports suggested an abdominal ultrasound would be better.
In a mere 12% (23/187) of cases was a significant abdominal pathology discovered on plain film. The main diagnosis was a small bowel obstruction in 13 cases (13/187; 7%). Other diagnoses included ingested foreign bodies, small bowel ischemia, sigmoid volvulus, and in one case, the incidental discovery of an abdominal aortic aneurysm.
 Dr. Toni Anderson.
Dr. Toni Anderson.As we all know, radiology is becoming an increasingly busy service worldwide. And although it may not be feasible to take a step backward and have all plain-film abdominal x-rays vetted prior to filming, such as is the case with CT and MRI, I wonder should there be better safeguards in place to avoid unnecessary scans. This would benefit patients and avoid the added healthcare costs attributable to imaging that is not indicated.
Also relevant here is that your article highlights the previous underestimation of radiation dosing of plain-film abdominal x-rays where obese patients are concerned as obesity, globally, is on the rise. My own study and the audit performed at Sandwell & West Birmingham are not the first nor will they be the last on this topic, and yet I wonder if the figures are ever going to improve simply by the use of educational postures and leaflets. Perhaps it should be engrained in junior doctors early in their careers. Or indeed should a higher threshold of vetting be instituted, perhaps by the radiographer performing the scan.
Dr. Toni Anderson is a junior doctor in Dublin who graduated in 2015, and is currently a trainee in general internal medicine. She completed a law degree at University College Dublin in 2009, and hopes to pursue a career in radiology from July 2019 after completion of basic specialty training in medicine.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.



















