A new audit of 200 consecutive requests for abdominal x-rays found that more than a quarter of referrals are wide of the mark, with general practitioners (GPs) being the worst offenders, delegates learned at this month's U.K. Radiological and Radiation Oncology Congress in Liverpool.
"Despite the presence of clear guidelines published by the Royal College of Radiologists (RCR), abdominal plain films are frequently requested with no appropriate indication, delivering an unjustified radiation (dose) to the patient, wasting resources, and providing false reassurance of negative signs," noted Dr. Rehaan Nensey, a radiologist at the Sandwell & West Birmingham Hospitals National Health Service (NHS) Trust in the U.K., and colleagues.
The researchers sought to evaluate the appropriateness of the abdominal x-ray requests according to the guidelines. Their target was that 100% of requests should meet the RCR's iRefer guidelines.
The group evaluated a total of 200 consecutive abdominal x-ray requests from different sites of the Sandwell & West Birmingham Hospitals NHS Trust within a 15-day period (1 to 15 January 2017) for their appropriateness with the iRefer guidelines, as outlined below:
- Acute abdomen with suspected bowel obstruction, indicated only in specific circumstances
- Acute exacerbation of inflammatory bowel disease or to monitor the condition
- Sharp/poisonous foreign body
- Smooth and small foreign body, such as a coin
- Blunt/stab abdominal injury, for which x-ray is not as reliable as CT but may be of use for detecting gross pneumoperitoneum
- Follow up calcium-containing renal calculi
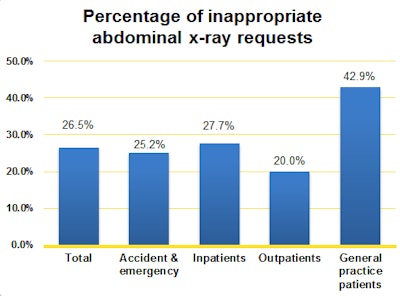
The team found that 53 requests (26.5%) did not meet the guidelines. The highest percentage of inappropriate requests (42%) came from GPs, while the lowest (20%) came from specialized outpatient departments. The researchers also found that 25.2% of accident and emergency requests and 27.7% of inpatient requests were noncompliant.
A total of 15 out of 53 inappropriate requests had follow-up imaging, and only three (5.7%) showed significant abnormalities. However, the abnormalities picked up by further imaging were themselves not indications for abdominal x-rays in the first place. This included one case of perforation and two cases of cholecystitis.
"The actual percentage of inappropriate requests is likely to be higher as the indication of bowel obstruction is often added, even if it is not consistent with the symptoms described," the authors noted in their e-poster presentation.
To address the problem, they recommended that educational posters be circulated throughout the hospital departments, including accident and emergency. These posters should contain examples of inappropriate and appropriate indications. In addition, they advocated that radiographers should be encouraged to discuss abdominal x-ray requests when they do not meet the RCR guidelines, and GPs must be sent leaflets and educational materials emphasizing the importance of requesting abdominal x-rays for the correct radiological examination for the indication, as per the iRefer guidelines.