A new computer-aided detection (CAD) algorithm for digital breast tomosynthesis (DBT) studies delivers high sensitivity and an acceptably low false-positive rate, according to Italian researchers. In a retrospective study of nearly 200 women who underwent DBT for breast cancer screening, CAD demonstrated sensitivity of 89% with a false-positive rate of 2.7 per breast.
"A digital breast tomosynthesis CAD system can allow detection of a large percentage (89%, 99 of 111) of breast cancers manifesting as masses and microcalcification clusters, with an acceptable false-positive rate," wrote Dr. Lia Morra, PhD, head of research at im3D, along with colleagues from the University of Turin and other institutions (Radiology, 11 May 2015).
DBT is an improvement over digital mammography in its ability to improve visualization of masses and architectural distortions more effectively and efficiently, they noted. It also diminishes the masking effect of superimposing glandular tissues. However, the fast-emerging modality may also present unique challenges for interpreting some lesions.
"Early reports showed that DBT might not be as effective for the detection of microcalcification clusters as it is for masses," making the search for microcalcification clusters more difficult and time-consuming than with digital mammography.
This gives CAD an opportunity to be especially helpful for DBT interpretation. Unfortunately, the few articles covering CAD and DBT are focused on the detection of masses and not on microcalcifications, Morra and colleagues wrote. So they designed a study that evaluated the performance of a commercial tomosynthesis CAD algorithm (CAD Breast DTS v2.2, research version, im3D) in an independent three-center cohort, measuring both sensitivity and specificity.
They tested the CAD algorithm retrospectively on a dataset of 175 patients, 123 of whom had histologically proven screen-detected breast cancers, and 52 of whom had normal results that included at least a year of negative results at follow-up. The datasets included craniocaudal and mediolateral oblique 2D mammographic and DBT views acquired with a commercially available DBT unit (Selenia Dimensions, Hologic).
The 123 patients with positive results had been examined in three different clinical centers. CAD results were assessed per lesion and by the number of false positives in patients with negative results.
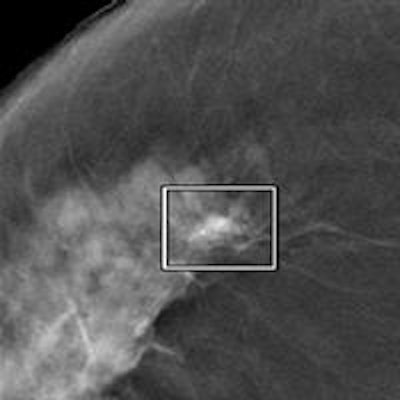
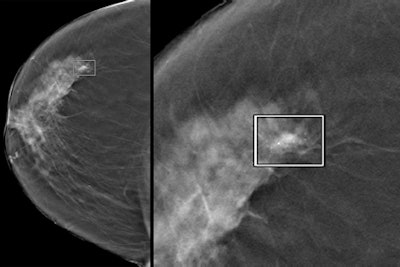 Left: A CAD-detected 12-mm invasive ductal carcinoma with associated microcalcifications. Right: A close-up of the tumor. Images courtesy of Dr. Giovanna Mariscotti from L'Azienda ospedaliero-universitaria San Giovanni Battista in Turin, Italy.
Left: A CAD-detected 12-mm invasive ductal carcinoma with associated microcalcifications. Right: A close-up of the tumor. Images courtesy of Dr. Giovanna Mariscotti from L'Azienda ospedaliero-universitaria San Giovanni Battista in Turin, Italy.High sensitivity, acceptable false positives
The results showed a total of 111 lesions were masses and/or microcalcifications (72 masses, 22 microcalcifications, 17 masses with microcalcifications) and 21 were architectural distortions. Lesions were annotated by radiologists who were aware of all available reports. CAD performance was assessed as per-lesion sensitivity and false-positive results per volume in patients with negative results.
Of the lesions detected, 62 of 72 were masses, 20 of 22 were microcalcifications, the authors wrote. Specifically, the CAD algorithm found 37 of 39 microcalcification clusters (95% sensitivity) and 79 of 89 masses (89% sensitivity), including 17 of 17 masses with calcifications. On average, 0.5 false positives per view were microcalcification clusters, 2.1 were masses, and 0.1 were masses and calcifications, the group reported.
The DBT CAD system allows for a large percentage of breast cancers manifesting as masses and microcalcification clusters, with an acceptable false-positive rate, but more studies with larger datasets and using equipment from different vendors will be needed to replicate the findings and understand the interaction of radiologists and CAD with DBT, they wrote.
"We envision that the role of CAD systems in DBT probably will be different; compared with full-field digital mammography, DBT yields superior diagnostic performance (both specificity and sensitivity) but poses additional challenges (mostly an increase in reading time), especially in organized reading programs," the authors wrote.
Mass margins are more clearly visible in DBT, but its 3D nature and the presence of artifacts due to acquisition angle complicates segmentation of both masses and calcifications. Processing 3D volumes also tends to create large numbers of false positives.
Among the study's limitations, most of the cohort came from a diagnostic rather than a screening population. The study did not assess benign lesions. Four-projection studies constituted only 63% of the cases, making it impossible to assess case-based false-positive rates, the authors wrote.
Still to come: CAD-radiologist interaction
Also, the CAD was applied by itself in a standalone manner; investigators did not study CAD-human interaction, which will need to be completed before screening can begin.
"While there have been several studies studying CAD-radiologist interaction for mammography CAD, there have been at the moment no attempts to study CAD-radiologist interaction with tomosynthesis," Morra wrote in an e-mail to AuntMinnieEurope.com. "We will certainly need to design and carry out future studies to study the effect of CAD on readers' performances."
The field of DBT CAD is very new, she added, and as a result the performance of CAD on its own will need to be more solid before embarking on studies of CAD-radiologist interaction. Several clinical trials are investigating the role of screening tomosynthesis, both in the U.S. and Europe. And the researchers have partnered with im3D in the Proteus Donna study, a two-arm randomized prospective trial comparing recall rate, detection rate, and interval cancers between double-reading digital mammography and double-reading DBT.
More than 50,000 screening subjects will be enrolled in the trial, making it one of the largest worldwide -- "and one of the few studies where tomosynthesis units from different vendors are included," Morra noted.
That trial will also pave the way for the use of CAD -- both alone and in conjunction with the reader -- in a screening scenario.