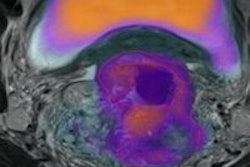
A multi-institutional study from Germany has joined a growing number of evaluations of tumor heterogeneity as a tool to assess cancer treatment responses. This study investigated textural parameters of tumor heterogeneity in F-18 FDG PET/CT images of patients with locally advanced rectal cancer, and adds further merit and validity of the use of tumor heterogeneity assessment to facilitate personalized oncologic therapy.
The study of 27 patients with rectal cancer revealed that the coefficient of variation (COV) --defined as the standard deviation of uptake divided by the mean uptake in the tumor volume -- showed a statistically significant capability to evaluate disease progression in patients receiving neoadjuvant radiation chemotherapy. COV also was used to identify patients with a high risk for disease progression and death.
PET has been used to assess tumor heterogeneity because it can visualize functional information directly, providing information about the surface structure of cells, receptor density, and cell metabolism. The study's lead author Dr. Ralph Bundschuh, a research scientist at the Universitätklinikum Bonn, and colleagues investigated the role of tumor heterogeneity in the assessment of therapy response on pretherapeutic F-18 FDG PET, as well as images recorded during and after therapy (Journal of Nuclear Medicine, June 2014, Vol. 55:6, pp. 891-897).
Three textural parameters were estimated within the tumor volume: the COV; skewness, a measure of the asymmetry of activity distribution in the lesion; and kurtosis, a measure of the peakedness of the activity distribution. All were assessed in 3D volumes. Five additional conventional parameters were used for comparison: maximum lesion diameter; morphologic volume of the lesion; maximum SUV (SUVmax); mean SUV (SUVmean); and total lesion glycolysis (TLG), the product of tumor volume and mean uptake.
The researchers performed receiver-operating characteristic (ROC) analysis to estimate optimal cut-off values for individual parameters for assessment of histopathologic response, disease progression, and survival for all investigated parameters, and also for changes in the parameters over the course of therapy.
Nineteen of the 27 patients, or 70.4%, responded to treatment based on histopathologic analysis. The parameters that showed a statistically significant predictive capability, as well as the highest values, were TLG, tumor volume, and COV. At optimal cut-off values, the sensitivity for predicting histopathologic response was 53% for TLG and tumor volume, and 47% for COV.
COV proved the best parameter for assessing early response, with a sensitivity of 68% and a specificity of 88%. A decrease of COV during and after therapy indicated histopathologic response. In fact, it was the only parameter to show a statistically significant predictive capability when changes in PET/CT images acquired before and two weeks after treatment were analyzed. COV also had the highest area under the curve for late response assessment, with a sensitivity of 79% and a specificity of 88%. TLG, skewness, kurtosis, and SUVmax were also statistically significant parameters.
In their analysis of parameters that may identify patients with a high risk of disease progression, Bundschuh and colleagues determined that COV also had the best predictive capability early in the course of therapy. Other parameters might have proved statistically significant predictors had more patients died or the patient cohort been larger.
The authors suggested that one reason for the correlation between a strong decrease in tumor heterogeneity during therapy and good therapy response and prognosis is that high heterogeneity may correspond to high levels of neovascularization, a characteristic of more aggressive tumors. They noted a decrease in tumor heterogeneity could be an indicator of reduced vascularization and necrosis. Consistent legion heterogeneity during therapy could indicate the presence of a tumor cell clone that does not respond to therapy.
Although the research team recommends additional research, they note COV is easy to calculate if the mean uptake and standard deviation within the tumor volume are known. They pointed out these parameters can be assessed with commercially available PET analysis software and could be used today in clinical routines. They recommend assessment of COV should be included in routine F-18 FDG PET/CT scans to identify patients responding to therapy, as well as patients with a high risk of disease progression.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.