Is the end in sight for sentinel lymph node biopsy (SLNB) for axillary staging of breast cancer patients? U.K. researchers call the procedure "redundant" in light of MR imaging with dye based on superparamagnetic iron oxide (SPIO).
SLNB is currently the standard of care for axillary staging of patients with breast cancer who have a clinically and radiologically negative axilla. Preoperative ultrasound with fine-needle aspiration (FNA) or core biopsy of abnormal lymph nodes is used to identify node-positive patients who can proceed directly to axillary lymph node dissection and thus avoid an additional unnecessary surgical procedure, according to an article published online in European Radiology (14 September 2013).
"However, the sensitivity of ultrasound-guided FNA/biopsy for the preoperative detection of axillary nodal metastases is variable with figures ranging between 25% and 97%," wrote Dr. Muneer Ahmed, from the department of research oncology at King's College London, and colleagues.
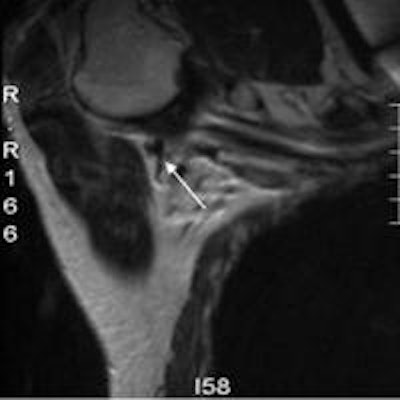
 An axillary MRI following the administration of subcutaneous SPIO into the breast (Endorem, Guerbet). The lymphatic tract is seen to go into a lymph node. Image courtesy of Mr. Michael Douek.
An axillary MRI following the administration of subcutaneous SPIO into the breast (Endorem, Guerbet). The lymphatic tract is seen to go into a lymph node. Image courtesy of Mr. Michael Douek.In addition, 34% of normal-appearing nodes are positive for malignancy, which begs the question of how best to target axillary nodes for core biopsy.
More intelligent targeting of the sentinel lymph node using ultrasound contrast agents such as microbubbles may be of benefit. Other techniques, such as ultrasound elastography, also have shown potential for preoperative axillary staging in breast cancer, especially considering the success of several studies, the researchers noted.
"However, in the current clinical context by using preoperative ultrasound staging of the axilla routinely, potentially up to 75% of patients will still have a negative SLNB and undergo an unnecessary invasive procedure with its associated morbidity," the researchers wrote. "Furthermore, ultrasound is of limited value for intraoperative localization of sentinel nodes in view of limited surgical ultrasound training and the limitations of using portable ultrasound machines to identify departmental radiological findings."
Ahmed and colleagues posit that noninvasive MRI options, such as axillary MRI, diffusion-weighted imaging (DWI), and SPIO-enhanced MRI, would be more useful. Specifically, data from studies using SPIO indicate that the technique has sensitivity and specificity for detecting axillary involvement of 98% and 96%, respectively.
SPIO injected interstitially into the periareolar region of the breast has been successfully used to guide SLNB. In a previous study, Johnson and colleagues showed 13 nodes containing metastases had variable quantities of iron within them, but the iron was not present in the areas of the node containing the metastasis (Histopathology, February 2013, Vol. 62:3, pp. 481-486).
Their study demonstrated that heterogeneous enhancement of sentinel lymph nodes and nonsentinel lymph nodes on contrast-enhanced MRI indicated a metastatic focus.
"This technique could potentially identify patients with significant axillary involvement preoperatively, who therefore require [axillary lymph node dissection]," Ahmed and colleagues wrote.
The current SentiMAG Multicentre Trial, a prospective phase II nonrandomized clinical trial comparing SLNB using a magnetic tracer and handheld magnetometer with the standard technique, will determine if the novel technique is viable in a larger patient cohort, they added. The trial has an MRI subprotocol to evaluate preoperative axillary MRI (with a magnetic tracer) for sentinel lymph node imaging and characterization.
"The findings of this preoperative imaging will then be correlated with the outcome of SLNB to determine the ability of SPIO-enhanced MRI to characterize the sentinel lymph nodes preoperatively," the researchers wrote. "However, this will be of limited clinical value since the CE Marked magnetic dye is not a contrast agent and can only be used to localize sentinel nodes."
Future contrast agents should further evaluate these findings, they added.
Also, the concept of selective axillary surgery could be used to identify and remove only involved axillary nodes, which would rely on improved preoperative imaging combined with novel techniques to guide surgeons intraoperatively to involved nodes. In this way, patients with a high clinical index of suspicion for axillary involvement could be offered further imaging, and those with a low index of suspicion, conservative management.
"The future for SPIO contrast-enhanced MRI is promising, and it is essential that funding is prioritized to include imaging trials and subprotocols to evaluate preoperative axillary MRI," the researchers concluded. "These trials will allow us to move forwards to a truly minimally invasive approach and individualized axillary management in breast cancer."



















