The use of routine follow-up ultrasound for early detection of nonpalpable locoregional recurrent cancer is advocated by South Korean researchers, writing in the 6 November issue of the European Journal of Radiology.
Even though locoregional recurrence occurs infrequently after mastectomy for breast cancer, screening ultrasound detects nonpalpable cancer before a clinical exam. And it's recommended that after patients have a mastectomy, they are physically examined every three to six months during the first three years, every six to 12 months during the fourth and fifth years, and yearly thereafter.
Imaging follow-up includes a yearly mammogram of the contralateral breast, but otherwise, "imaging modalities have not been widely used for examining the scar and axilla after mastectomy and axillary dissection, because recurrent tumors involving the chest wall or skin are frequently detected during clinical examinations," according to Dr. Jin Hwa Lee from Dong-A University in Busan, South Korea, and colleagues (European Journal of Radiology, 6 November 2012, article in press).
The researchers sought to determine the value of screening ultrasound when detecting nonpalpable locoregional recurrence following mastectomy for breast cancer, and to describe the ultrasound appearances of recurrent cancers.
Of the 468 patients assessed in their retrospective study, 19 (4.1%) showed suspicious for malignant nodules using ultrasound screenings at mastectomy sites and ipsilateral axillary fossae. Of the suspicious lesions, 10 were malignant, and one false-negative case was identified.
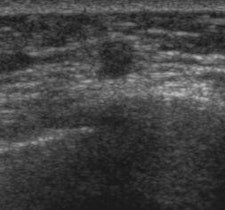
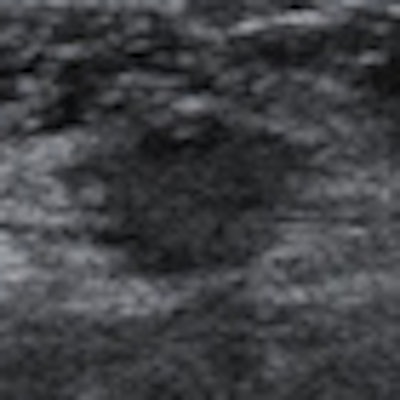
 Left: A 47-year-old asymptomatic woman who had undergone a mastectomy. Ultrasound shows a 5-mm round mass with uncircumscribed margins and mild hypoechogenecity at the deep muscle layer of the mastectomy site. Right: A 45-year-old asymptomatic woman who had undergone a mastectomy. Ultrasound shows a 10-mm irregular hypoechoic mass with not-circumscribed margins at the deep muscle layer of the mastectomy site. Recurrent ductal carcinomas were confirmed by a ultrasound-guided core-needle biopsy in both cases. Images courtesy of Dr. Jin Hwa Lee.
Left: A 47-year-old asymptomatic woman who had undergone a mastectomy. Ultrasound shows a 5-mm round mass with uncircumscribed margins and mild hypoechogenecity at the deep muscle layer of the mastectomy site. Right: A 45-year-old asymptomatic woman who had undergone a mastectomy. Ultrasound shows a 10-mm irregular hypoechoic mass with not-circumscribed margins at the deep muscle layer of the mastectomy site. Recurrent ductal carcinomas were confirmed by a ultrasound-guided core-needle biopsy in both cases. Images courtesy of Dr. Jin Hwa Lee.Ultrasound screening had a sensitivity of 90.9% and a specificity of 98%. A biopsy-positive predictive value of 52.6% was demonstrated. Cancer detection rates were 2.1% with ultrasound screenings of mastectomy sites and ipsilateral axillary fossae.
The common ultrasound features were irregular shape, uncircumscribed margins, and hypoechoic masses with intratumoral vascularities. The most common location was within the deep muscle layer, Lee and colleagues wrote.
"Current guidelines recommend a clinical follow-up of the mastectomy site and the ipsilateral axilla, with imaging only performed as a second-line measure," the researchers wrote. "However, clinical examination may not be sufficient for recurrent lesions located deep within soft tissue or beneath a postoperative scar."
Occult recurrent cancers at the mastectomy site are located mostly in subcutaneous fat and deep muscle layers, not in the skin, which would allow for easy detection at clinical examinations, they added. The false-negative rate of physical examinations of axillae has been reported to be as high as 39%.
"Routine mammographic imaging is technically limited in patients who have undergone mastectomies; therefore, it has not generally been advocated, and its sensitivity in the detection of recurrent tumors is inferior to that of clinical examination," they wrote. "Ultrasound is a useful imaging method that can overcome the limitations and discomfort associated with a mammogram in this clinical situation, and it has been known to be useful for the diagnosis of postoperative complications and for guiding fluid aspirations."
The American College of Radiology (ACR) BI-RADS guidelines have been proposed for detection and diagnosis of breast lesions in normal, untreated breasts, but there are no specific guidelines for lesions in a mastectomy site, the researchers noted. In previous studies, all hypoechoic nodules in the mastectomy site were considered as suspicious on ultrasound -- i.e., BI-RADS category 3 lesions in native breast tissue were classified as BI-RADS category 4 lesions in mastectomy sites because some studies reported recurrent lesions have probably benign features on ultrasound.
"The great technical advances in ultrasound instruments in the recent decade may enable better detection and characterization of focal nodules," the researchers wrote. "Moreover, in Asian countries, radiologists have much experience of using ultrasound diagnosis due to a high annual volume of bilateral whole-breast ultrasound procedures."
The researchers speculated that BI-RADS final assessments can be applied to lesions at mastectomy sites if done carefully.
"When a nodule was oval-shaped, circumscribed marginated, isoechoic, or mildly hypoechoic without any intratumoral vascularity, it was classified as a probably benign finding, corresponding to BI-RADS category 3," they wrote. "We considered rounded nodules or focal nodules with not-circumscribed margins or with any intratumoral vascularity on color power Doppler US as BI-RADS category 4."
The researchers admit that while ultrasound screenings are valuable in detecting clinically occult locoregional recurrences after mastectomy for breast cancer, there are potential problems, including unnecessary short-term follow-up, benign-result biopsies due to false-positive results, false-negative results, and excessive cost and physician time.
Despite the limitations, the researchers conclude that routine follow-up ultrasound should be employed, and applying the BI-RADS category can be valuable in differentiating between benign and malignant nodules.