Surgical management of breast cancer often includes lumpectomy or mastectomy, followed by breast reconstruction. Each of these types of reconstruction has different appearances on MRI, and knowing what to look for is critical in the interpretation of MRI following surgery, according to a major article published in Insights into Imaging.
Researchers at Beth Israel Deaconess Medical Center in Boston reviewed different types of breast reconstruction following cancer surgery and described expected imaging appearances and complications seen in reconstructed breasts when imaged with MRI (Insights into Imaging, 16 March 2012, online first).
"Historically, imaging reconstructed breasts has not been typical," lead author Dr. Vandana Dialani told AuntMinnieEurope.com. "But with screening MRI, we've started seeing more reconstructed breasts on imaging and it's important to differentiate what's normal from what's not to avoid unnecessary procedures."
Postmastectomy reconstruction with a tissue expander and implant happens in stages, she noted. Once expansion is completed and the patient is cleared for another operation, the second stage of reconstruction is performed. Implant-based reconstruction may be combined with acellular dermal matrix coverage or with a lattisimus dorsi flap. But acellular dermal matrix coverage does not enhance with gadolinium, and it will appear as overlying the implant, filling the gap between the skin and the implant.
The latissimus dorsi flap is a standard method for breast reconstruction, and is often combined with a tissue expander or implant (for a thin patient with a small breast volume, the technique can be used alone as the primary reconstruction without an implant), Dialani's team wrote. On MR images, the flap has a "tailed" appearance in the lateral breast, due to its overlying skin and fat flipped and tunneled from the back to and from the reconstructed breast tissue.
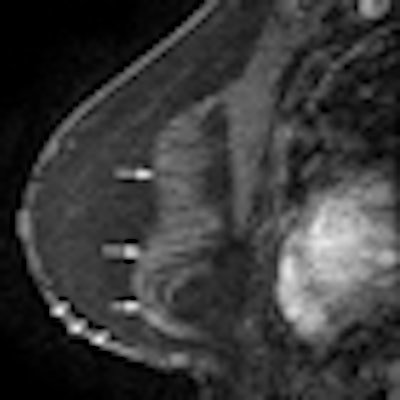
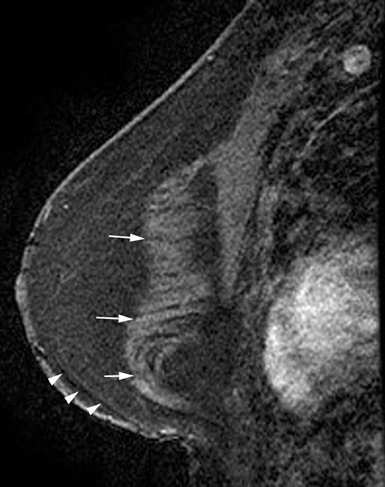 Reconstruction with latissimus dorsi myocutaneous flap: Latissimus dorsi muscle, fat and skin are rotated to reconstruct the breast. Top: Sagittal fat-saturated T1-weighted image shows latissimus dorsi muscle flipped anteriorly for reconstruction (white arrows) and the denuded dermal layer is seen parallel to the chest wall (white arrow heads). Bottom: Axial fat-saturated T1-weighted subtraction image with postcontrast gadolinium injection, the flap consisting of the latissimus dorsi muscle and its overlying skin and fat flipped and tunneled from the back to the neobreast (white arrow), giving a tailed appearance to the muscle in the lateral breast. This can be used as a differentiator on imaging from transverse rectus abdominis myocutaneous (TRAM) flap reconstruction. All images courtesy of Dr. Vandana Dialani.
Reconstruction with latissimus dorsi myocutaneous flap: Latissimus dorsi muscle, fat and skin are rotated to reconstruct the breast. Top: Sagittal fat-saturated T1-weighted image shows latissimus dorsi muscle flipped anteriorly for reconstruction (white arrows) and the denuded dermal layer is seen parallel to the chest wall (white arrow heads). Bottom: Axial fat-saturated T1-weighted subtraction image with postcontrast gadolinium injection, the flap consisting of the latissimus dorsi muscle and its overlying skin and fat flipped and tunneled from the back to the neobreast (white arrow), giving a tailed appearance to the muscle in the lateral breast. This can be used as a differentiator on imaging from transverse rectus abdominis myocutaneous (TRAM) flap reconstruction. All images courtesy of Dr. Vandana Dialani.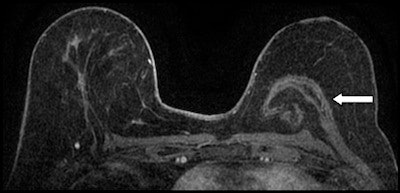
Transplanting a transverse rectus abdominis myocutaneous (TRAM)flap is a commonly used surgical procedure for breast reconstruction following mastectomy. For the technique, surgeons harvest the rectus abdominis muscle, along with the subcutaneous soft tissue. There are pedicled TRAM flaps, which take their blood supply from the superior epigastric vasculature, and there are free TRAM flaps, which take their blood supply from the inferior epigastric artery and vein, Dialani and colleagues wrote.
Common markers of TRAM flap reconstruction include lower abdominal fat in place of normal glandular tissue of the breast and atrophied rectus abdominis muscle along the anterior chest wall; in this technique, the bulk of the flap is usually in the center on the MR image, especially on the axial images.
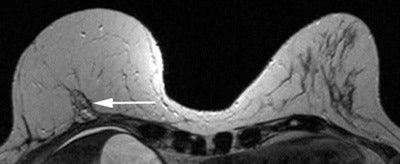 Pedicled TRAM flap-rectus abdominis muscle rotated up to the chest for breast reconstruction. Axial nonfat saturated T2-weighted images with dynamic gadolinium injection, showing the atrophied rectus abdominis muscle along the anterior chest wall (white arrow) and the bulk of the muscle in the center as against the eccentric location in the latissimus flap. The lower abdominal fat constitutes the right reconstructed breast. Normal left breast is shown for comparison.
Pedicled TRAM flap-rectus abdominis muscle rotated up to the chest for breast reconstruction. Axial nonfat saturated T2-weighted images with dynamic gadolinium injection, showing the atrophied rectus abdominis muscle along the anterior chest wall (white arrow) and the bulk of the muscle in the center as against the eccentric location in the latissimus flap. The lower abdominal fat constitutes the right reconstructed breast. Normal left breast is shown for comparison.Other characteristics of reconstructed breast tissue can include fibrosis -- a common result of radiation therapy in the breast; atrophy and fibrosis often appear in women who have had breast reconstruction.
"One of the challenges in evaluating the postoperative breast is to differentiate between postoperative or postradiation therapy scarring and tumor recurrence," the authors stated. "Here MR imaging may often prove helpful, as postradiation therapy fibrosis often displays low signal intensity on T2-weighted images."
Another benign complication to watch for is fat necrosis, which is a common complication of TRAM flap reconstruction, they wrote. At MRI, fat necrosis manifests as a round or irregular mass (with central high-signal intensity on nonfat-suppressed unenhanced T1-weighted images and high signal on T2-weighted images); it shows variable enhancement with gadolinium, as well as fast initial enhancement and washout on the delayed enhancement images.
Finally, MRI is a sensitive method for detecting ruptured implants: Signs such as the linguine (collapsed and folded elastomer shell floating in gel) and keyhole (silicone on both the inside and outside of a radial fold) have been well documented.
What should radiologists look for to find cancer that returns? At MRI, tumor recurrence following lumpectomy is characterized by a mass with low signal intensity on T1-weighted images, low to intermediate signal intensity on T2-weighted images, and rapid enhancement following gadolinium contrast administration. Features like rim enhancement and spiculated morphology also increase the likelihood of malignancy, the authors wrote.
Knowing how breast reconstruction surgery is conducted is key to reading MR images, Dialani told AuntMinnieEurope.com.
"Once you understand how the surgery is done -- and how to recognize complications related to surgery -- you can interpret the MR images better," she said.



















