The U.K. Royal College of Radiologists (RCR) has published new recommendations on breast cancer screening and symptomatic breast imaging that reflect the continuing demand for examinations as a result of changes in the provision of cancer services in the National Health Service (NHS) and the widespread development of specialist breast clinics.
"The document is provided for radiologists and other members of breast teams providing diagnostic, treatment, and follow-up services for patients with symptomatic breast problems, explained Dr. Pete Cavanagh, dean of the RCR's Faculty of Clinical Radiology. Guidance on the role of imaging in breast cancer screening also is included.
The document (3rd edition, ref No: BFCR[13]5), which can be downloaded free of charge from the RCR website, is an update of the previous RCR's "Guidance on Screening and Symptomatic Breast Imaging, Second Edition," which is now withdrawn. It does not include guidance on topics already covered in the "Best practice diagnostic guidelines for patients presenting with breast symptoms" from the U.K. Department of Health.
A screening trial for women between the ages of 70 and 73 and 47 and 49 is underway now in England and Wales. There is currently no evidence to support routine screening of women older than 70, and for women between the ages of 47 and 49, meta-analysis of randomized, controlled trials have shown a mortality benefit of 17%, which is significantly less than that seen when screening women between the ages of 50 and 69, the authors stated.
"Those studies demonstrating the largest mortality reductions have used short screening intervals (12 to 18 months) and multiple screening rounds (five or more). The low breast cancer incidence coupled with the high percentage of female deaths due to breast cancer in this age group provokes debate regarding the importance of screening younger women," they noted.
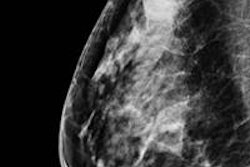
Two-view digital mammography at each screening visit is recommended, but screening more frequently than every year is not advocated.
Women using long-term hormone replacement therapy (HRT), particularly estrogen and progesterone combined, are at an increased risk of breast cancer and breast cancer death, according to the guidelines. The effect is seen in pre- and postmenopausal women, and though the effect is largely resolved within two years after discontinuing HRT, both sensitivity and specificity of mammography are reduced in women taking HRT. Baseline mammography is not routinely required prior to commencing HRT.
Ultrasound on its own is not an effective method for routine screening, the authors noted. Its use as an adjunct to mammography in screening women with high mammographic density is associated with an increase in detection of early breast cancer and a reduction in the interval cancer rate, but it has a poor specificity. In early studies, shear-wave elastography shows promise in improving the specificity and sensitivity of breast ultrasound, but further multicenter studies are required, they explained.
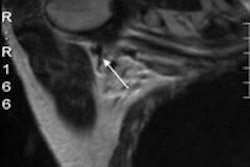
Breast MRI has advantages, such as high sensitivity for invasive (but less so for in situ) disease, and may be useful in local staging prior to breast conservation in women with invasive lobular cancer or dense breasts, as well as when there is discordance between assessments of tumor size using different methods, added the authors. MRI is also useful for monitoring response to neoadjuvant chemotherapy and detecting occult primary tumors in women presenting with adenocarcinoma in axillary lymph nodes, and it's the modality of choice to assess the integrity of breast implants.
An appendix to the document covers professional standards and requirements for radiologists involved in symptomatic breast imaging. A radiologist must be personally involved in the interpretation and reporting of at least 500 symptomatic mammograms per year. Those participating in breast screening should undertake a minimum of 5,000 screening and/or symptomatic cases a year.
Cavanagh acknowledged the help of Dr. Andrew Evans, professor of breast imaging at Ninewells Hospital in Dundee, in updating this guidance.
For further details about this document, visit the RCR website.