Left ventricular (LV) diastolic dysfunction is surprisingly common in cardiovascular MRI (CMR) examinations-- even in apparently healthy individuals -- and more prevalent among men than women, according to research from Portugal published online on 3 August in European Radiology.
In 48 asymptomatic volunteers, a group from the University of Coimbra found LV diastolic dysfunction in 20% to 24%, depending on how it was measured. The prevalence was higher in men regardless of the criteria used.
Diastolic dysfunction can increase the risk of heart failure, the authors explained. Diastolic heart failure is characterized by impaired LV relaxation, increased LV stiffness, increased insterstitial deposition of collagen, and alterations in extracellular matrix proteins. But CMR's accuracy, combined with new postprocessing tools, makes it the best modality to measure diastolic function.
"Measurement of diastolic function is clinically feasible in a single CMR exam," wrote Dr. Bruno Graça, Dr. Maria João Ferreira, and colleagues. "The prevalence of diastolic dysfunction is higher in men than in women."
The condition accounts for up to half of all heart failure cases "and has a prognosis which is as ominous as that of systolic HF (heart failure)," they noted. As a result, clinicians place a lot of emphasis on the timely detection of subclinical LV systolic and diastolic dysfunction as risk factors for heart failure.
In recent years, echocardiography has given ground to CMR, which has become the gold standard for LV diastolic assessment due to its high spatial and temporal resolution, image quality, and lack of geometric limitations on imaging.
"Flow analysis with CMR allows the quantitative assessment of blood velocity, with the advantage that the tomographic plane of interest can be positioned optimally in a larger area than in Doppler echocardiography," Graça and colleagues wrote.
"CMR provides velocities (meters per second) as well as volume flow (milliliters per second) and is less operator- and angle-dependent" than ultrasound, they wrote.
But despite CMR's accuracy and flexibility, few studies have used the modality to study LV dysfunction at CMR. This study examined the prevalence of LV dysfunction in a population without known heart disease, defining reference values and gender differences.
The cohort of 48 volunteers (19 men and 29 women, mean age 49 ± 7 years, mean weight 68 ± 11 kg with normal LV ejection fraction) had no history of heart disease, and normal ECG. Patients with signs of systemic inflammation or valvular disease, among other conditions, were excluded.
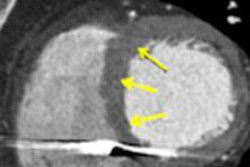
CMR was performed on a 3-tesla system (Magnetom Trio, Siemens Healthcare), acquiring cardiac cine images with steady-state free-precession images and retrospective gating, with participants supine and performing a breath-hold, the authors wrote. Two-dimensional flow-sensitive phase-contrast gradient-echo sequences were used for velocity-encoded (VENC) MRI flow measurements perpendicular to the orifice of the mitral valve. VENC-MRI slices were acquired at the tip of the mitral valve leaflets, and quantitative image data analysis was performed using Segment dedicated software (Medviso).
The prevalence of LV diastolic dysfunction varied between 20% (based on evaluation of LV filling profiles) and 24% (based on the evaluation of the transmitral flow), the group reported.
The indexed LV myocardial masses at end diastole were significantly greater in men than in women (p = 0.038). Indexed left atrial (LA) minimum and maximum volumes were also significantly greater in men (p = 0.046 than in women (p = 0.032). Indexed LV end-diastolic and stroke volumes were significantly greater in men than in women (p = 0.007 and p = 0.005, respectively). In addition, indexed LV myocardial masses at end diastole were significantly greater in men than in women (p = 0.038).
Similar gender-based differences were seen in left auricular measures, with indexed LA minimum and maximum volumes significantly greater in men (p = 0.046) than in women (p = 0.032).
Finally, peak filling rates (PFR) were significantly larger in men than in women (p = 0.043) although PFR values indexed to end-diastolic volume and stroke volume were comparable, the authors wrote. PFR normalized to end-diastolic volume (EDV) less than 2.5 EDV per second was considered abnormal.
Men led in diastolic dysfunction, with a higher prevalence than that of women, independent of measurement criteria (p 0.004 to 0.022).
"Indexed LV end-diastolic volume, indexed LV stroke volume, indexed LV mass, indexed LA minimum volume, and indexed LA maximum volume were all significantly greater in men than in women (p < 0.05)," they stated. All ejection fraction measurements were normal.
All nonindexed LA volumes were significantly higher in men, except for the left atrial emptying fraction, according to Graça and colleagues.
"While these differences disappeared in most normalized parameters, indexed LA minimum and maximum volumes remained higher in men," the group wrote, noting that the findings are in line with a previous study by Hudsmith et al, who reported higher absolute LA volumes in male patients with similar ejection fraction in both genders.
Age might account for the higher LA maximum volumes in men, and gender differences in LA minimum volumes may result from the reduced ejection force of the atrial pump in men, the group wrote.
MRI technology has caught up to the task of measuring volumes, making it a good choice for assessing diastolic dysfunction. LV filling profiles have been used in other modalities, specifically radionuclide cineangiography and SPECT, but such applications in CMR have been impractical in the past due to the need for extensive manual planimetry across all temporal phases, which "would typically require tracing of more than 200 images per patient," they wrote.
Improvements in postprocessing tools now enable semiautomatic segmentation of all phases, quickly providing the "time-varying course of the LV volume" during the cardiac cycle, the researchers wrote.
LA volume index greater than 34 mL/m2 is an independent predictor of death, heart failure, atrial fibrillation, and ischemic stroke, they noted. However, dilated left atria are sometimes seen in patients without diastolic dysfunction, including patients with "bradycardia and four-chamber enlargement, anemia and other high-output states, atrial flutter or fibrillation, and significant mitral valve disease," Garça and colleagues wrote.
To compensate, this study used high cutoff values that eliminated most of the confounding conditions.
The study underscores the feasibility of using a single CMR exam to study left heart volumes and function, including diastolic flow and LV filling data, the group wrote.
Identifying impaired LV diastolic function in adults is clinically important considering the high risk of the condition in patients.
"[O]ur observations provide promising initial results for the routine use of CMR to study the prevalence and gender differences in subclinical LV diastolic dysfunction," the researchers wrote.