Late-enhancement CT can replace MRI for preprocedural evaluation of myocardial scar in patients with ventricular tachycardia (VT), according to a study from Italy. That's good news, the researchers said, because CT actually needs to replace MRI for preprocedural planning in many VT patients who have contraindications to MRI.
In more than 30 patients who had VT but could not undergo MRI, late-enhancement CT showed subepicardial enhancement suggestive of postmyocarditis scars, postischemic scars, and transmural involvement, the study team reported at the 2013 ECR. Meanwhile, electroanatomic mapping (EAM) confirmed low-voltage areas that late-enhancement CT had identified in 85% of cases with a full or partial match. Radiofrequency ablation (RFA) was performed within the late-enhancement regions.
Ventricular tachycardia occurs when myocardial scars from infarction or replacement fibrosis in structural cardiomyopathies provide a substrate for re-entry of the electrical current, leading to life-threatening arrhythmias. Implantable cardioverter-defibrillators (ICD) are often implanted to prevent sudden death, said Dr. Caterina Colantoni from the San Raffaele Scientific Institute and Vita Salute University in Milan, in her presentation.
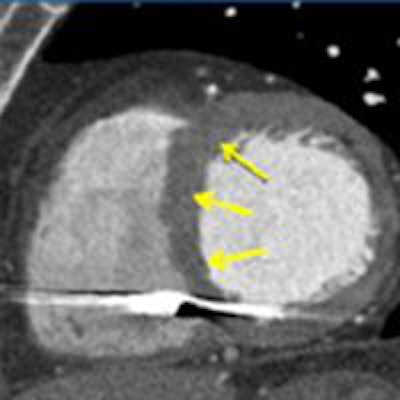
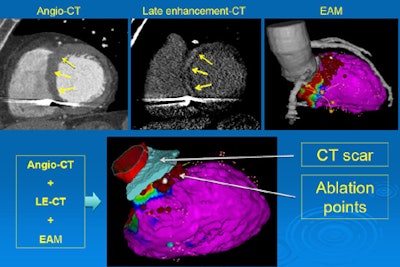 Coronary CTA images (left) show myocardium, and myocardial scar substrate in late-enhancing multidetector CT images (center), and electroanatomic mapping (EAM) image (right). Three image datasets combined (below) show myocardial scar guiding determination of ablation points. Images courtesy of Dr. Caterina Colantoni and Dr. Antonio Esposito.
Coronary CTA images (left) show myocardium, and myocardial scar substrate in late-enhancing multidetector CT images (center), and electroanatomic mapping (EAM) image (right). Three image datasets combined (below) show myocardial scar guiding determination of ablation points. Images courtesy of Dr. Caterina Colantoni and Dr. Antonio Esposito.ICDs don't solve the arrhythmia problem, of course, so radiofrequency therapy ablation is used as the primary therapy for VT. Planning for RFA is usually performed using EAM to map the substrate myocardial scar and guide RF catheter ablation. But the procedure has several limitations, including low anatomic resolution, a lack of information about epicardial fat and the course of epicardial vessels, as well as false detections of low-voltage areas.
As a result, MRI is the gold-standard modality for preprocedural planning with RFA, as it provides a ventricular anatomic wall map, superior contrast resolution, and 3D information about tissue substrate characterization.
"Unfortunately, the presence of ICD is a problem, because from 70% to 80% of patients have ICD, and most of them are not MRI-compatible ... MRI-compatible ICDs produce artifacts," Colantoni said. "So the purpose of our study was to detect and characterize myocardial scars in patients with recurrent episodes of ventricular tachycardia, with late-enhancement, and compare our findings with electronic mapping."
In all, 34 patients underwent 64-detector multidetector CT (Brilliance, Philips Healthcare) before EAM and RFA. The protocol included CT angiography and a low-energy delayed scan 15 minutes after injection of high-concentration nonionic contrast. Of the 120 mL contrast, 30 mL were injected immediately after CTA for the late-enhancement scan.
Prospectively gated ECG-triggered CTA was performed in 18 patients with heart rates < 65 bpm following beta-blocker administration, using a step-and-shoot protocol, and subsequent axial scans triggered in the mid-diastolic phase (40% and 80% of the RR interval)
Retrospectively gated CTA with dose modulation was performed in eight patients with heart rates that remained above 65-bpm after beta-blocker administration, with subsequent axial scans performed in the mid-diastolic phase (75% of the RR interval). Padding was adjusted from 0-150 ms. Images were uploaded to a workstation using Carto-Merge software (Biosense Webster) for anatomic support.
"We evaluated late-enhancement location that could be subendocardial, subepicardial, or transmural," Colantoni said. Segmental distribution of scars at imaging was compared with anatomic mapping according to the 17-segment model of the American Heart Association.
CT results showed:
- 10 patients with subepicardial scars in a postmyocarditis pattern
- 22 patients with subendocardial or transmural scars in a postischemic pattern
- One patient with a large fibroadipose substitution of subepicardial left-ventricle myocardium suggesting left-dominant arrythmogenic cardiomyopathy
- One patient had no scars at imaging
Scars at EAM were located within the areas of late enhancement in 16/35 patients (47%). There was a partial match between imaging findings and EAM was seen in 14 patients (41%), and no matching was found in four patients (12%).
"The RF ablation points were always located within the scars identified at imaging or along the edge of the late enhancement area in all 30 patients," she said. The study had a few limitations, including a small, heterogeneous patient population, and there was no pixel-by-pixel comparison of the images with the EAM, she said.
"We can say that CT with late enhancement was very useful in the detection and characterization of the scar substrate in tachycardia in patients with ICD," Colantoni said. "The sites of RF ablation were always within the scar areas identified by late-enhancement CT, and so it could be used to plan and guide electroanatomic mapping and RF ablation and to suggest the best approach to mapping" -- endocardial versus epicardial.
In response to questions from the session moderators, Colantoni said the next phase of the study would evaluate the effectiveness of RFA in the patients who were treated based on CT guidance. She also acknowledged that artifacts from cardiac devices obscuring the left-ventricular junction can still be an issue with CT as well as MRI -- to the point where a handful of cases with no match between CT and EAM may have been affected by artifacts.
Reached by email, lead author Dr. Antonio Esposito offered more information about CT artifacts encountered in the imaging technique.
"The electrocatheters from the ICD create some streak artifacts (visible in the images) that typically involve small portions of the inferior septum and of the inferolateral wall of the left ventricle," Esposito told AuntMinnieEurope.com. "These artifacts are more evident in the late-enhancement phase due to the use of low kV, and may be responsible of the loss of some small scar in these segments. However, as demonstrated by our study, cardiac CT with the late-enhancement phase provides good results for the assessment of scar substrate in patients with recurrent ventricular tachycardia, also in the presence of ICD."
Moreover, the researchers consider CT to be the only possible option in patients with ICD, because a large percentage of ICDs are not MR-compatible and also, in patients with MR-compatible devices, the ICD-electrocatheters create very large high-intensity artifacts that often completely obscure all anterior and anterolateral segments of the left ventricle, Esposito said.
"So ICDs are still considered a contraindication to cardiac MR imaging or significantly affect cardiac MR imaging quality, with subsequent very poor assessability," he said. "Factors potentially affecting image quality of [late-enhancement CT] study regards the patients' characteristics and in particular the ability of patients to collaborate with breath-holding and the patients habitus with important quality deterioration in obese patients."



















