The internal carotid artery (ICA) is the intracranial artery to pick for arterial input function (AIF) calculations following CT perfusion imaging of stroke patients, according to a new study in European Radiology.
Dutch researchers reported that the choice of artery to plug into AIF calculations makes a difference in perfusion accuracy, and that ICA was the most reliable vessel for the role when scanning with wide-area-detector CT, though differences between the arteries were small. In addition, eliminating the venous outflow function (VOF), though technically possible with today's wide-area multidetector-row CT (MDCT) scanners, is a bad idea.
"In 256-slice MDCT, selecting the ICA as the AIF and continuing the use of a venous sinus as the VOF will improve the accuracy" of CT perfusion, wrote Dr. Joris Niesten, Dr. Irene van der Schaaf, and colleagues from University Medical Center Utrecht (Eur Radiol, May 2013, Vol. 23:5, pp. 1242-1249).
An essential tool
CT perfusion has become essential for evaluating cerebrovascular diseases, especially ischemic stroke, assessing vascular support for tumors, and guiding reperfusion therapy.
The technology has a lot in its favor, offering generally low costs and wide availability where it's needed. But questions remain regarding the validity of the perfusion data, which guide critical patient care decisions, Niesten and colleagues wrote.
"An important problem resulting in reduced accuracy and reproducibility is the selection of the ... AIF and venous output function, with a reported variability in interobserver agreement between 10% and 27 %," they wrote. "Since definitions of salvageable and irreversible tissue, the vascular support of tumors and delayed cerebral ischemia are based on absolute perfusion values, the pursuit of quantitative [CT perfusion] remains relevant."
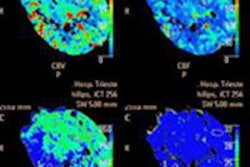
Choosing the AIF and the VOF are needed to create quantitative maps showing cerebral blood volume, cerebral blood flow, and mean transit time, the study authors noted.
Cerebral blood volume is the ratio of the area under the time-enhancement curve of the first passage through the tissue to the area under the curve of the first passage of contrast through the artery chosen as the AIF, with a correction factor to account for differences between small and large vessels.
Choosing small vessels as the AIF can produce partial-volume effects that potentially underestimate the area under the AIF curve. The VOF is used to correct for these partial-volume effects. A noniterative deconvolution method is applied to create a mean transit time.
Varying opinions on the validity of values from different arteries mean that no consensus has been reached as to which artery should be selected as the AIF, the researchers wrote.
Among the few studies that address the choice of artery for AIF, most focus on the difference in perfusion measurements between an artery with or without an upstream occlusion, and advise use of the artery without an occlusion, the group wrote.
On the other hand, some investigators advise selecting the artery as close as possible to the region of interest of the tissue, whereas other studies recommend to using the anterior cerebral artery or even an extracranial vessel as AIF, the researchers noted.
Wider anatomic coverage in today's scanners mean that the large ICA and basilar arteries can be chosen as the AIF, reducing the influence of partial-volume effects and improved quantitative perfusion values, they wrote, so much so that VOF may no longer be needed for partial-volume correction.
The purpose of the study was to evaluate the accuracy and reproducibility of quantitative perfusion by the assessment of the optimal artery for the AIF and re-evaluating the necessity of the VOF, the authors wrote.
Niesten and colleagues examined 44 ischemic stroke patients (mean age 71 years, range 45-97 years) who underwent nonconstrast CT as well as CT perfusion and CT angiography with MDCT. Nearly half of the thrombi (45%) were located in the right middle cerebral artery.
Noncontrast and CT perfusion images were acquired on a 256-slice CT scanner (Brilliance iCT, Philips Healthcare). Nonenhanced CT settings included 120 kVp and 300 mAs, with reconstruction of 5-mm slices and collimation settings of 128 x 0.625. CT perfusion images were acquired using 80 kVp, 150 mAs, and 5-mm reconstructed slice thickness following injection of 40 mL of contrast (300 mg I/mL) at 6 mL/sec, followed by a 40-mL saline flush, the study team wrote.
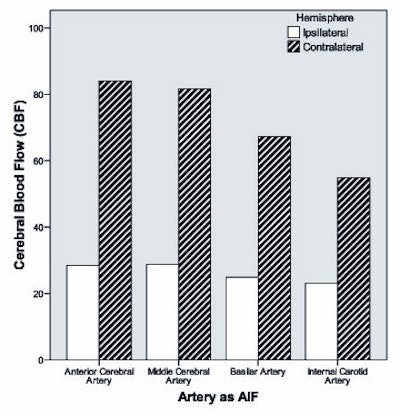
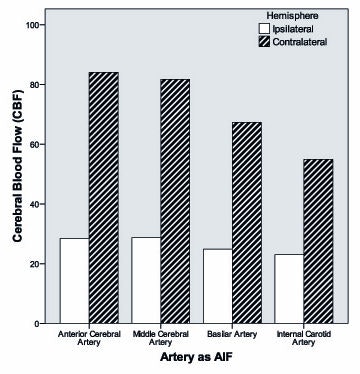
The authors chose four arteries: the anterior cerebral artery, the middle cerebral artery, internal carotid artery, and basilar artery as the AIF. Then they analyzed the resulting area under the time-enhancement curve of the AIF (AUCAIF), as well as quantitative perfusion measurements using analysis of variance and the paired t test.
Reproducibility was examined by deleting the VOF and comparing perfusion measurements with and without it using a paired t test. Both the AUCAIF and perfusion measurements resulting from using the different AIFs revealed significant differences between them (all p < 0.0001).
"The ICA had the largest AUCAIF and resulted in the highest mean transient time and lowest cerebral blood flow, whereas the basilar artery showed the lowest cerebral blood volume," they wrote.
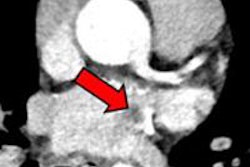
 AUCAIF of different cerebral arteries. All images courtesy of Dr. Joris Niesten.
AUCAIF of different cerebral arteries. All images courtesy of Dr. Joris Niesten.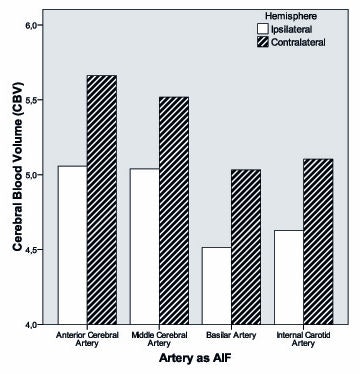
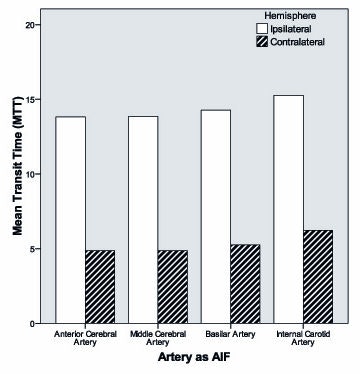
The VOF could not be dispensed with. Not using it produced significantly higher cerebral blood volume and cerebral blood flow in two-thirds of patients on the ipsilateral (p < 0.0001 for cerebral blood volume, p < 0.007 for cerebral blood flow) and contralateral hemisphere (p < 0.0001 for cerebral blood volume, p < 0.019 for cerebral blood flow).
"The choice of which artery to select as the AIF has significant effects on the accuracy of quantitative perfusion measurements, leading to significant and major differences" of up to 13% in mean transient time, 25% in cerebral blood volume, and 50% for cerebral blood flow, Niesten and colleagues reported.
Using the internal carotid artery for AIF delivers optimal perfusion values, while eliminating the venous output function would have a negative effect on validity, they wrote.
This study shows that when wide-area CT technology is used, the ICA produces the most appropriate AIF compared with other intracranial arteries, the authors wrote, noting that previous research showed that greater z-axis coverage with 256-slice MDCT provides more diagnostic CT perfusion information to work with.
As for study limitations, different software packages produce considerably different CT perfusion measurements, though the Philips software used for this study did offer the advantage of a time-sensitive algorithm, and to further mitigate any effects of delay, the group chose vessels that were less affected by it.
Still, further study is needed on other algorithms, the group wrote. Also the effect of different algorithms on infarct core/penumbra maps and on clinical decision-making as a result needs more research.