SAN FRANCISCO - A U.K. practice found that for chest pain patients with low amounts of heart calcium, high-definition (HD) CT provides little benefit. But high-risk patients or those with pre-existing disease might benefit, according to a study at this week's International Society for Computed Tomography (ISCT) meeting.
Because of the global recession, there's been a shuffle in how cardiac patients are worked up in the U.K. In the past, physicians took patient history, determined the type of pain, risk factors, age, and sex of the patient, then conducted an exercise test, made a diagnosis, followed by either further investigation or treatment. Now, the U.K. National Institute for Health and Clinical Excellence (NICE) has told cardiologists to abandon the exercise test, because "it's a waste of time," according to Dr. Carl Roobottom from the Peninsula Radiology Academy in the U.K.
Instead, cardiologists are to assess the patient's symptoms: typical angina, atypical angina, and nonspecific chest pain, then assess the patient's risk. From there, the patient is divided into three groups: high-risk patients go to cardiac cath, intermediate-risk patients go to functional imaging, and low- to intermediate-risk patients go to CT.
"That's good news for CT because it's the first time it placed CT in the diagnostic algorithm," Roobottom said.
CT didn't get a higher rank because although it demonstrates high sensitivity and specificity, its positive predictive value (PPV) varies. Also, a number of clinical trials excluded patients with high calcium scores, according to a NICE assessment.
NICE suggested that if a patient has a calcium score below 400, they get a CTA; if the patient has a calcium score above that, they get a cardiac cath because CTA can't cope. "We all know why," Roobottom said, "because we don't have enough spatial resolution and we get problems with blooming artifact."
But high-definition CT, with its higher resolution, could offer a solution. The scanner's gemstone detector is much faster in response to when a photon hits it, according to Roobottom.

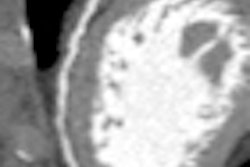
 Image series shows comparison images demonstrating how high-definition CTA improved reporting accuracy. Case is a 49-year-old man with previous stent to the circumflex artery with recurrent pain. Left: Image shows a stent in the circumflex artery but no stenosis. Right: Image shows an occluded right coronary. All images courtesy of Dr. Carl Roobottom.
Image series shows comparison images demonstrating how high-definition CTA improved reporting accuracy. Case is a 49-year-old man with previous stent to the circumflex artery with recurrent pain. Left: Image shows a stent in the circumflex artery but no stenosis. Right: Image shows an occluded right coronary. All images courtesy of Dr. Carl Roobottom."My analogy would be a conventional detector is like an energy-saving light bulb, so we turn it on and off very quickly, [and] you still get some light in the background, whereas the gemstone is a bit more like a flashlight so acts like a strobe," he said.
The HD CT system (Discovery HD 750, GE Healthcare) can run either in conventional mode or HD, which wobbles the focal spot in the x and y axes. HD works well, but as voxel size goes down, images will get more noisy. That's why iterative reconstruction (IR) works in tandem with HD because it helps to counteract that noise, Roobottom said.
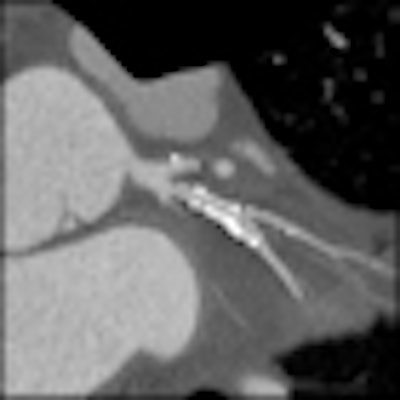
 Same patient as above. Image shows the circumflex but demonstrates how use of the Discovery HD750 scanner allows clear visualization of the short stenosis despite the stent and high level of calcium in the arteries.
Same patient as above. Image shows the circumflex but demonstrates how use of the Discovery HD750 scanner allows clear visualization of the short stenosis despite the stent and high level of calcium in the arteries.At Roobottom's institution, they run the HD scanner in both modes depending on the calcium score. Low calcium scores receive conventional imaging, while high calcium scores receive HD imaging.
"Does it work? It certainly gives us more confidence," Roobottom said. During his ISCT presentation, he illustrated several cases in which multiple stenoses were identified that "might have been missed" if the HD setting hadn't been used. HD also identifies stents, native vessels, and reduces blooming artifacts.
The most impressive part of HD scanning, however, is the exclusion of patients who have lots of calcium, according to Roobottom. "About half the patients who've got calcium scores above 400 don't require further investigation when we do them on our HD scanner," he said.

 Same patient as above. Left: A conventional left coronary angiogram confirming the CT findings. Right: A conventional right coronary angiogram confirming findings.
Same patient as above. Left: A conventional left coronary angiogram confirming the CT findings. Right: A conventional right coronary angiogram confirming findings.Since introducing the HD scanner, the radiologists are not only conducting NICE's recommendations, but they're also getting a lot of referrals from cardiologists -- cardiologists send patients with established disease for stent assessment because the radiologists can give more accurate results because of HD.
"It causes some logistical problems for us because we have one HD scanner and three non-HD scanners," Roobottom said. "Patients who've got high calcium scores ... have to physically get off our non-HD scanner and put them on the HD scanner to get the benefits."
But HD has some disadvantages. Because of the small focal spot, radiologists are limited to 800 to 830 mA and limited in the size of patients they can scan, and there is also high image noise.
"What's going to happen is there's going to be a shift of patients from functional imaging to more anatomical imaging," he predicted.