CT coronary artery calcification (CT CAC) is proving effective for triaging patients who have presented at the rapid access chest pain clinic in a leading U.K. hospital. Based on six years of experience, the technique may now be more useful than traditional assessment methods.
Initial evaluation of patients with nonacute chest pain has traditionally involved calculation of pretest probability, consideration of cardiovascular risk factors, resting 12-lead ECG, and an exercise treadmill test before further stress imaging or invasive coronary angiography. However, the U.K. National Institute for Health and Clinical Excellence (NICE) published guidelines last year, and they recommended using CT CAC as a first-line diagnostic tool in stable chest pain patients with a pretest probability (PTP) of between 10% and 29%.
"CT CAC is a low radiation dose and relatively inexpensive technique that can be provided as a rapid service in busy imaging departments," noted authors from the Chest Pain Clinic at Harefield Hospital in Harefield, U.K., in a poster presentation at the European Society of Cardiology (ESC) 2011 annual congress in Paris.
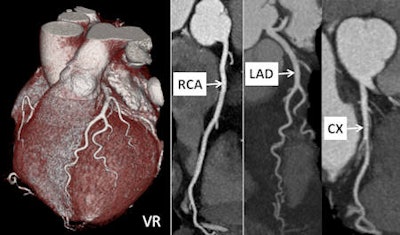 Dual-source cardiac CT in a 55-year-old woman suffering from atypical chest pain. The CT examination was performed using a prospective ECG-triggered cardiac sequence mode (tube voltage 100 kV, tube current time product 200 mAs), resulting in a radiation dose estimate of 1.2 mSv for the examination. Volume-rendered image (VR) on the left and curved reconstructions of the right coronary artery (RCA), left anterior descending artery (LAD), and circumflex artery (CX) demonstrate adequate image quality and absence of relevant coronary stenosis. Image courtesy of Dr. Sebastian Leschka, Zurich University Hospital.
Dual-source cardiac CT in a 55-year-old woman suffering from atypical chest pain. The CT examination was performed using a prospective ECG-triggered cardiac sequence mode (tube voltage 100 kV, tube current time product 200 mAs), resulting in a radiation dose estimate of 1.2 mSv for the examination. Volume-rendered image (VR) on the left and curved reconstructions of the right coronary artery (RCA), left anterior descending artery (LAD), and circumflex artery (CX) demonstrate adequate image quality and absence of relevant coronary stenosis. Image courtesy of Dr. Sebastian Leschka, Zurich University Hospital.The research team, led by Dr. N. Bhatia and cardiology nurse consultant Alison Pottle, examined the use of CT CAC and compared it with traditional methods for predicting coronary artery disease (CAD). Patients who presented between October 2003 and March 2010 with nonacute chest pain and no prior history of CAD were retrospectively reviewed. All patients were categorized according to their PTP, using the Duke's criteria based on the type of chest pain and risk factors, as recommended by the NICE guidelines.
Eligible patients had exercise ECG. All men older than 40 years and all women older than 50 years underwent CT CAC. Invasive angiography was performed on the basis of PTP, results of exercise ECG, CT CAC, and myocardial perfusion scintigraphy. Patients were considered to have significant CAD if they underwent percutaneous coronary intervention or coronary artery bypass grafting. The predictive value of PTP, exercise tolerance testing, and CT CAC for significant CAD was determined using multivariable logistic regression analyses and their areas under the receiver operating characteristic (ROC) curves.
The study population comprised 791 patients (394 men and 397 women, average age 59) with no CAD and who had complete risk factor information available. Of the total, 326 (39.6%) had hypertension, 85 (11.2%) had diabetes, 315 (40.5%) had dyslipidemia, and 138 (17.4%) were smokers. The chest pain type was typical in 190 (24%) cases, atypical in 560 (70.7%) cases, and noncardiac in 41 (5.1%) cases, according to the authors.
Overall, 85 patients (10.1%) were in the very low PTP category, which was defined as being below 10%, while 212 (26.8%) patients were in the low category of 10% to 29%. A total of 222 (28%) patients fell into the intermediate category of 30% to 59%, and 272 (34.3%) were in the high category of 60% to 90%.
CT CAC was performed in 705 patients. Almost 48% of patients had absent CAC in the entire study group, and significantly more patients had absent calcification in the very low and low PTP groups, stated Bhatia. Of the patients, 150 (21.3%) went to have invasive angiography based on clinical/imaging criteria, and 40 patients were found to have significant CAD. Of the patients who underwent invasive angiography, 18 had a CT CAC of zero, one of whom with high PTP had significant CAD. None of the patients with low or intermediate PTP and absent CT CAC (n = 10) had significant CAD.
In the authors' multivariate model adjusted for age, sex, hypertension, hyperlipidemia, smoking, diabetes, PTP, abnormal CT CAC, and exercise ECG positivity, the important independent predictors for having significant CAD were PTP, abnormal CT CAC, and exercise ECG positivity. However, exercise ECG was inconclusive for patients unable to exercise in 46% of cases, they wrote.
The sensitivity and specificity were 96% and 51%, respectively, for CT CAC, and 35% and 94%, respectively, for ex-ECG. The positive predictive value was 12% for CT CAC and 32% for ex-ECG, while negative predictive value was 95% for both techniques.
"In patients with stable chest pain presenting to the clinic, PTP, CT CAC, as well as exercise ECG where performed, are strong independent predictors of significant CAD," they concluded. "CT CAC can be performed in patients irrespective of their exercise capacity and resting ECG changes. Absence of CT CAC, particularly in those with low to intermediate pretest probability, correlated with absence of significant CAD."
For further reading, the authors referred ESC attendees to JS Skinner's NICE guidance "Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin" in Heart (June 2010, Vol. 96:12, pp. 974-978).