Perfusion CT with a 320-detector-row scanner offers improved resolution of pancreatic tumors due to its ability to image the entire organ without slice overlap, according to researchers from Berlin and Toronto.
Pancreatic tumors visualized on the 320-detector-row system show significantly lower perfusion compared to surrounding normal tissue. The researchers are hopeful that whole-organ perfusion CT of the pancreas will prove its value not only for evaluating malignancy and resectability -- daunting tasks under the best circumstances -- but also for monitoring treatment response.
Although perfusion CT of the pancreas has shown promise in previous studies, image quality has been generally poor because CT scanners that acquire data in slices that are then reconstructed into volumes are limited to acquiring "only selected levels" of the organ, "and with breathing motion this results in slice mismatch," said Dr. Sonja Kandel from Charité Hospital in Berlin and the University of Toronto.
"With 320-slice CT, you now have 16-cm [of anatomic coverage] and we can examine the entire pancreas," she said. "But there is still the problem of image registration due to breathing differences," which must be corrected via image processing.
The study, which Kandel presented at the 2009 RSNA meeting in Chicago, aimed to evaluate a whole-organ perfusion protocol in patients with primary pancreatic cancers using 320-detector-row CT -- and to analyze perfusion differences between normal and diseased pancreatic tissue, Kandel said.
The researchers examined 40 patients with proven primary pancreatic cancer on a 320-detector-row CT scanner (Aquilion One, Toshiba Medical Systems, Otawara, Japan). Before scanning, all patients were given oxygen hyperventilation through a mask to support longer breath-hold sequences.
The dynamic CT protocol consisted of 15 intermittent low-dose scans acquired within 90 seconds. The protocol began with a noncontrast scan to determine that the entire pancreas would be covered in the 16-cm scan field. Following contrast injection at 8 mL/sec and dynamic intensity measurements in the left ventricle, scanning (100 kV, 40 mAs, 320 x 0.5 mm) was started manually, Kandel said.
The researchers then used a maximum slope technique to calculate perfusion at the pancreas head, tail, and body. Next, they generated core perfusion maps and used a Kruskal-Wallis test to determine normal distribution, she said.
The results in all 40 cases showed normal pancreatic tissue perfusion values ranging from 0.54 to 1.81 min-1, while perfusion of pancreatic tumors varied from 0.08 to 1.38 min-1. The researchers were able to correct for all motion artifacts, and in all cases perfusion of the pancreatic tumor at 0.06 to 1.38 min-1 was significantly lower compared to the pancreas head at 0.19 to 1.87 min-1, as well as compared to the body and tail (p < 0.001), Kandel said.
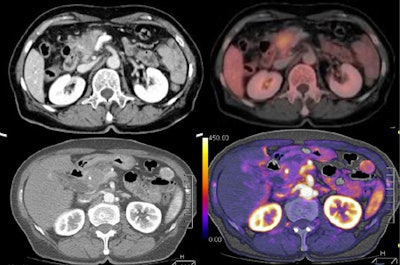 |
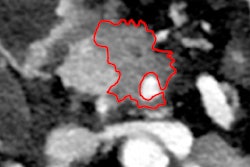
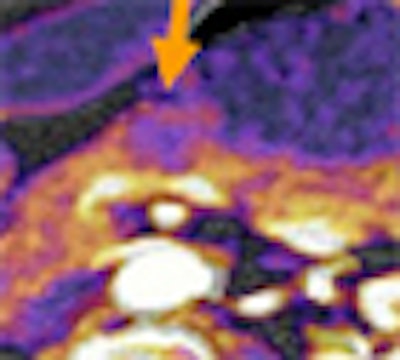
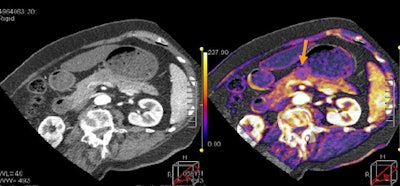
| Tumor and pancreas head are visible on tumor map, with PET image for comparison. All images courtesy of Dr. Sonja Kandel. |
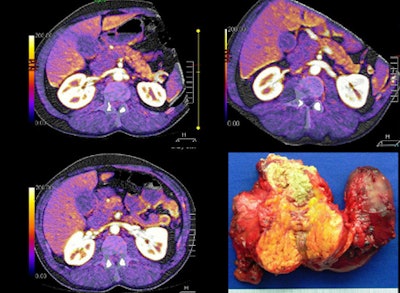 |
| Large pancreatic mass and head are visible at perfusion CT, with surgery specimen for comparison. |
 |
| Small 2-cm mass in the body of the pancreas, clearly imaged on the perfusion map. |
"Perfusion values were lower in the head, corpus, and tail, and there was only a small difference between head, corpus, and tail values," Kandel said.
The study had several limitations, including the exclusion of patients with tumors smaller than 2 cm, Kandel said. And the reference standard for the perfusion measurements was suboptimal.
"We had no comparison to the pathological or gold standard, and we used pancreatic tissue as an internal reference for each patient, so we don't know if the tumor affected the pancreatic tissue," she said.
Dynamic imaging with 320-detector-row CT permits the assessment of whole-organ perfusion in the pancreas, and clearly shows perfusion differences between primary pancreatic carcinoma and normal pancreatic tissue, Kandel concluded. Perfusion CT "may serve as a valuable tool to monitor therapeutic response in patients with pancreatic cancer," Kandel said.
By Eric Barnes
AuntMinnie.com staff writer
February 5, 2010
Related Reading
Perfusion CT handily distinguishes malignant neck nodes, January 25, 2010
FDG-PET/CT trumps CT in detecting anal carcinoma, November 25, 2009
PET/CT directs head and neck cancer treatment, November 17, 2009
Axillary ultrasound can help avoid sentinel node biopsy surgery, October 8, 2009
ROI changes colorectal tumor perfusion measurements, August 26, 2008
Copyright © 2010 AuntMinnie.com