LONDON - In a suspected case of acute pancreatitis, it's essential to use CT at the right time, a Dutch expert told delegates at the British Institute of Radiology (BIR) annual conference on Friday.
"Do not perform CT on day one. You can unintentionally fool the clinician," said Dr. Thomas Bollen, a radiologist from St. Antonius Hospital, Utrecht. "A CT is best performed at least 72 hours after symptom onset."
He illustrated his point with an example of a patient who was assumed to have interstitial disease when a CT scan was carried out on day one, but was found to have extended necrosis of the pancreas on day three. The patient subsequently died on day five.
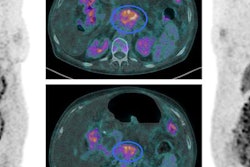
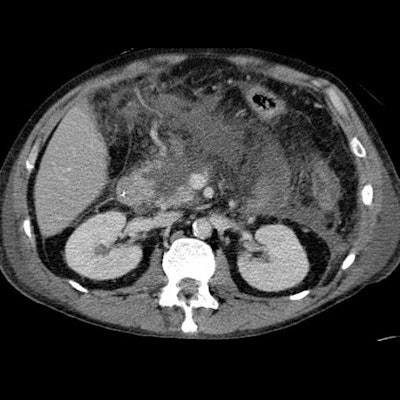
 When you see a peripancreatic collection, then describe where it is and outline its characteristics in detail. Clinical images courtesy of Dr. Thomas Bollen.
When you see a peripancreatic collection, then describe where it is and outline its characteristics in detail. Clinical images courtesy of Dr. Thomas Bollen."The day-one scan fooled the clinicians big time. This is often the case. We should only perform a CT scan when we suspect a patient of having a severe complication, such as bowel ischemia, or if there is diagnostic uncertainty," Bollen emphasized. "If a patient cannot tell you that they have abdominal pain because they are unconscious, but they have elevated enzymes, then they need a CT to confirm the diagnosis."
Timing and careful interpretation of CT scans is important in acute pancreatitis, and you must never assume anything, he added.
"In acute pancreatitis, describe what you see, rather than jumping to conclusions," Bollen said. "If you see nonenhancement areas, then describe the location and extent, and if you see a peripancreatic collection then describe where it is and its characteristics in detail."
Rising incidence
Incidence of acute pancreatitis has increased by 75% since the late 1990s, with the majority (80%) of cases due to gallstones and alcohol use. There are around 4,000 admissions in the Netherlands annually, from a population of 17 million. In severe pancreatitis (20% of the total), approximately 40% of patients can develop infected necrosis, and this has 20% to 30% mortality, he explained.
Based on the Revised Atlanta Classification from 2012, there are two morphologic types of acute pancreatitis: interstitial edematous pancreatitis and necrotizing pancreatitis. Furthermore, there are four types of associated pancreatic collections. Early collections (< 4 weeks) are called either acute peripancreatic fluid collection or acute necrotic collection. Late collections (> 4 weeks) are called either pseudocyst or walled-off necrosis.
 About two-thirds of patients with infected necrosis must be treated surgically.
About two-thirds of patients with infected necrosis must be treated surgically.Collections can be tiny and discrete and at other times they can be extensive, and CT is not very effective at identifying the exact content of a collection in or around the pancreas, according to Bollen.
"It is often a mixture of fluid, fat, necrosis, or hemorrhage, but CT generally displays it as fluid," he said. "It is also crucial to note the presence of pancreatic necrosis, whether collections are present or not, and to describe any gas bubbles, degree of encapsulation, or hemorrhage."
Misinterpreting collections is a common error, Bollen noted, pointing out there are many reports where collections have been misread as a pseudocyst or an abscess.
"In doing this, the radiologist has already interpreted the collection and it gives the clinician the impression that it could be fluid only. But actually, if you performed an MRI on these patients you would find that many of these patients have necrosis, which is a whole different ball game," he commented.
 Dr. Thomas Bollen from Utrecht.
Dr. Thomas Bollen from Utrecht.Infected necrosis needs to be treated surgically in about two-thirds of patients, and if drainage is performed on an area with necrosis, the patient might not improve and surgery is ultimately required to remove the necrotic material. If the patient is on a clinical ward rather than a surgical ward, the surgeon might be introduced too late to the patient, resulting in delay of appropriate treatment, Bollen said.
Imaging in acute pancreatitis is not without its pitfalls, he continued. In particular, central gland necrosis, a subtype of necrotizing pancreatitis, is important because it enables valuable prognostic information on a day-three scan.
"If I see a patient with midgland necrosis and significant remaining viable pancreatic tail, I tell the surgeon or clinician that this patient has a high chance of intervention somewhere during the course of their disease. In more than 90% of these patients, increasing collections are observed on serial CTs that require intervention," Bollen noted.
Finally, he explained that central gland necrosis is associated with pancreatic duct disruption, especially if the necrosis extends over two centimeters.