A German study has found that cardiovascular MR changes clinical management in approximately two-thirds of heart patient cases, and the modality can also eliminate the need for additional imaging procedures.
The results from the European Cardiovascular Magnetic Resonance (EuroCMR) registry also indicate that cardiovascular MR with contrast is safe and produces diagnostic-quality images in 98% of cases. The study, led by Dr. Oliver Bruder, was published online August 12 by the Journal of the American College of Cardiology.
The EuroCMR registry enrolled 11,040 consecutive patients between April 2007 and January 2009. The sample was divided into two groups: 3,475 patients who underwent cardiovascular MR stress testing and 7,565 patients who did not.
The most important clinical indications for the scans were myocarditis and cardiomyopathies, risk stratification in suspected coronary artery disease and ischemia, and assessment of viability. Some 88% of patients received gadolinium-based contrast agents, while 21% underwent adenosine perfusion, and 11% received high-dose dobutamine stress cardiovascular MR.
|
||||||||
| Source: EuroCMR |
Before undergoing cardiovascular MR, the vast majority of patients received transthoracic echocardiography (64%) or underwent cardiac catheterization (25%). The remaining patients received either transesophageal echocardiography, cardiac CT, or SPECT imaging. For 23% of the patients, cardiovascular MR was the first imaging procedure they received.
The researchers defined severe complications as death, resuscitation, or any other condition related to the cardiovascular MR procedure that required inpatient monitoring for at least one night after the MR scan for conditions such as allergic shock and arrhythmias. Post-MR complications such as dyspnea, chest pain, allergic reactions without shock, or problems related to intravenous lines were defined as mild.
Cardiovascular MR complications
In their review, the researchers found that approximately 99% of all cardiovascular MR procedures (10,896 scans) were performed without complications. Mild complications occurred in 124 patients (1%), while severe complications occurred in only five patients (0.05%). The most common mild events were dyspnea, chest pain, and extra systoles, which occurred during dobutamine or adenosine infusion (76% of the mild cases), followed by mild allergic reactions after injection of contrast (22% of mild cases).
Five patients were afflicted with severe complications. The researchers found one case of nonsustained ventricular tachycardia and one case of ventricular fibrillation during dobutamine infusion. Two cases of heart failure occurred, and there was one case of unstable angina related to adenosine stress. All severe complications were related to stress testing. There were no deaths during or due to cardiovascular MR.
Patient management
The study defined a change of patient management as cases in which the MR scan resulted in a new diagnosis that was not suspected before, or if the scans resulted in a change in medication or invasive procedures, such as coronary angiography or surgery, immediate hospital admission, or discharge from a hospital.
In 61.8% of the cases (6,822 patients), the authors wrote, cardiovascular MR had a "direct impact ... on the clinical management by providing an unsuspected new diagnosis (16.4%) and/or resulting in therapeutic consequences."
The study also determined that "good image quality" was achieved among 9,938 (90%) patients. In 897 cases (8%), image quality was considered moderate but was still of diagnostic quality. Poor, nondiagnostic image quality occurred among 189 (2%) patient cases.
 |
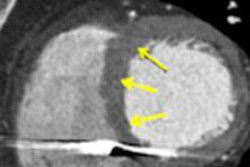
| Adenosine perfusion cardiac MR scan shows stress-induced ischemia in several coronary artery territories without myocardial scarring or wall motion abnormalities. Stress perfusion defects in the left anterior descending and right coronary artery are shown by the white arrows. Images courtesy of EuroCMR and JACC. |
The researchers also noted a "significant trend toward poorer image quality" in patients older than 75 years of age, compared to patients younger than 45 years. "Despite this decrease of image quality with age," the authors wrote, "the ability of cardiovascular MR to derive a diagnosis and the impact on patient management was not affected. In fact, the percentage of therapeutic consequences was even significantly higher in older patients compared with younger patients."
In the patient sample, cardiovascular MR alone was sufficient to avoid additional noninvasive imaging procedures in 9,494 patients (86%). Among the patients who received cardiovascular MR as their first imaging procedure, 8,832 (80%) patients required no additional imaging procedures.
Study limitations
Among the limitations of the study, the researchers noted that patients did not undergo systematic clinical follow-up, and, "thus, theoretically possible cases of nephrogenic systemic fibrosis may have been missed despite the fact that our mean dose of contrast media was low (1.28 mmol/kg), and we did repeatedly contact the participating centers but did not receive any reports of nephrogenic systemic fibrosis."
Because most complications of stress cardiovascular MR are not related to cardiovascular MR imaging itself, but to stressing the patient, stress cardiovascular MR is likely to be as safe as stress echocardiography, stress nuclear testing, or even obtaining a simple treadmill electrocardiogram (approximately one fatal complication or myocardial infarction in 2,500 cases).
As for the clinical implications of the study, the researchers said that the increased routine use of cardiovascular MR could reduce the number of invasive procedures and SPECT scans in the future. Echocardiography will probably remain the first-line cardiac test due to its speed, flexibility, and low cost, but cardiovascular MR could become valuable in the further workup of patients, the authors concluded.
By Wayne Forrest
AuntMinnie.com staff writer
September 25, 2009
Related Reading
CMS OKs MRI blood-flow coverage, July 2, 2009
Cardiac MR techniques improve myocardial assessment, June 15, 2009
MRI detects bleeding in the heart after a heart attack, February 13, 2009
MRI can provide safe imaging for pediatric heart patients, August 29, 2008
MRI evaluation of chest pain cuts acute coronary syndrome, August 15, 2008
Copyright © 2009 AuntMinnie.com