
New studies appearing in Radiology online examine two different etiologies associated with myocardial fat deposits. Their presence on imaging studies, both in CT and MRI, can help radiologists evaluate the extent of disease and potential risks.
First, a CT study examines myocardial fat deposits as a potential component of tuberous sclerosis complex (TSC), an autosomal dominant neurocutaneous disorder characterized by tumorlike malformations involving many organ systems, including the brain, kidneys, and skin.
In the second study published online before print, MRI was used to evaluate myocardial fat deposition after left ventricular myocardial infarction.
Congenital tuberous complex
In practice at University Medical Center Utrecht in the Netherlands, which specializes in the treatment of TSC, physicians noticed focal areas of fat within the myocardium in the basal portions of the heart in abdominal CT screening exams, according to Dr. Miraude Adriaensen, Dr. Cornelia Schaefer-Prokop, and colleagues.
However, TSC's "classic triad of seizures, mental retardation, and facial angiofibromas" occurs in fewer than half of all patients, the group wrote. To facilitate diagnosis, a clinical scoring system was developed that required the presence of two major features (facial angiofibromas or forehead plaques, shagreen patch, hypomelanotic macules, etc.) in addition to two minor features (Radiology, published August 2009 before print).
Aiming to potentially improve diagnosis, the authors examined the morphologic characteristics of the foci in 55 patients with known TSC (mean age, 37 years; range, 16-67). Another group of 55 patients without the disease were used as a control group.
The retrospective study included patients with CT images available that included at least the basal portions of the heart. CT images were examined for areas of fat attenuation in the depicted portions of the myocardium.
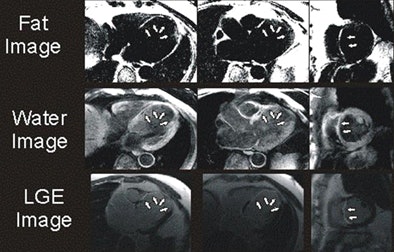
The study revealed foci of fat attenuation within the myocardium in 35 (64%) of 55 patients with TSC. Ranging in size from 3 x 1 mm to 62 x 31 mm, the fat was well circumscribed and focal. The majority of foci were found in the interventricular septum and left ventricle wall, with a few others in the right ventricle wall and papillary muscles.
"This location differs from intramyocardial fat in the right ventricle that has been described in healthy patients and in patients with arrhythmogenic right ventricular dysplasia (ARVD)," they wrote.
In addition, ARVD patients show a more diffuse fat infiltration as opposed to the focal mainly ovoid fatty foci seen in TSC patients in the study, they noted. No enhancing regions were seen in the fatty foci in TSC patients, in contrast to foci seen in patients with primary cardiac hemangioma.
 |
| Myocardial fat in patient with tuberous sclerosis complex at CT. Image courtesy of Dr. Miraude Adriaensen. |
Only one individual in the control group (34-year-old woman) had a thin curvilinear hypoattenuated lesion in a subendocardial location, which might be suggestive of prior myocardial infarction.
"Despite incomplete depiction of the heart with CT, the majority of patients with TSC demonstrated well-circumscribed foci of fat attenuation in the myocardium that were not present in age- and sex-matched control subjects," Adriaensen and colleagues wrote. "This suggests that such fatty foci may be another characteristic of TSC."
MRI for postinfarction myocardial fat deposition
Another study in Radiology online found a high prevalence of fat deposition at MRI near areas of chronic myocardial infarction, further elucidating an association that has been previously found, both clinically and in autopsy studies. In one study, as many as 84% of myocardial scars associated with chronic ischemic heart disease showed fatty replacement.
The authors examined the prevalence of fat deposition in myocardial infarction (MI) using MR fat-water separation imaging.
Dr. James Goldfarb and colleagues from State University of New York at Stony Brook and St. Francis Hospital in Roslyn, NY, also looked at the relationship between left ventricular (LV) fat deposition and myocardial scar characteristics, in addition to regional and global cardiac functional parameters.
The "association between right ventricular myocardial fibrosis and fat is unclear regarding its origin, significance, or even clinical usage," the authors wrote. "Although the patient population, clinical manifestation, and treatment of arrhythmogenic right ventricular dysplasia and LV MI differ greatly, detection of both left and right ventricular fat and fibrosis could benefit from the use of similar imaging strategies (Radiology online, published July 2009 before print).
 |
| Above, four-chamber, three-chamber, and short-axis images of a patient with fat deposition in segments of myocardial infarction. Precontrast fat-water separation imaging shows midwall fat deposition that is hyperintense in fat images and hypointense in water images. Late gadolinium-enhanced (LGE) infarct imaging shows an apical-septal chronic myocardial infarction. Below, fat-water separation imaging color overlay. Colored fat displayed on grayscale water images from two patients with chronic myocardial infarctions. Arrows point to midwall fat deposition. Images courtesy of Dr. James Goldfarb. |
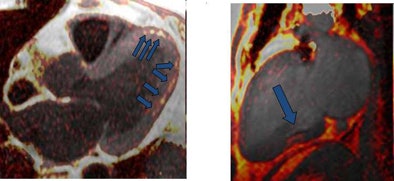 |
The study examined 25 patients with LV MI (mean age, 64.3 years; range, 43.2-82.1 years) using a 1.5-tesla MRI scanner system. Protocols included volumetric cine, fat-sensitive, and late gadolinium-enhanced (LGE) infarct imaging. Water-fat separation was performed by using a three-point Dixon reconstruction from in- and opposed-phase black-blood gradient-echo images.
The authors compared fat deposition location with LGE infarct using a 17-segment model. They compared global and regional functional variables, LGE volumes, and fat deposition using the Pearson correlation, Student's t-test, and multiple regression techniques.
Fat deposition was seen in 68% of patients in areas of chronic MI. Patients with fat deposition on imaging had larger infarctions (30.0 mL ± 15.1 [standard deviation] versus 14.8 mL ± 6.1; p = 0.002), less wall thickening (2.3% ± 20.0 versus 37.8% ± 34.4; p = 0.003), and impaired endocardial wall motion (2.9 mm ± 2.0 versus 5.8 mm ± 2.6; p = 0.007) compared to normal patients, the group reported. In addition, the volume of fat deposition correlated with infarct volume, LV ejection fraction, LV end-diastolic volume index, and LV end-systolic volume index.
The authors found no significant difference between the groups with and without LV fat deposition with regard to subject age, infarct age, body mass index, or body surface area.
"Since fat deposition was found solely in myocardial segments with or directly adjacent to MI, one might infer that LV MI is a precursor to LV myocardial fat deposition," Goldfarb and his team wrote, adding that serial imaging over several years would be necessary to test the hypothesis. "We also found that fat deposition was predominately midmyocardial or midepicardial, whereas results of prior autopsy and CT studies suggest that fat deposition almost always affects the subendocardium."
MRI is uniquely suited to the study of fat deposition "owing to its sensitivity to the off-resonance properties of fat, allowing fat-water separation imaging and the viewing of MI in all stages" using late gadolinium-enhanced imaging, combined with fat-water separation.
Previous studies have demonstrated significant increases in lipid content after brief coronary occlusion and reperfusion, which can be detected by MR as well as nuclear imaging techniques. Lipid accumulation can represent a symptom of MI or a precursor to MI, as metabolism changes from fatty acids to carbohydrates such as glucose, they wrote.
"There is a high prevalence of fat deposition in healed MI. It is associated with postinfarction characteristics including infarct volume, LV mass, wall thickness, wall thickening, and wall motion," the authors wrote.
The factors leading to fat deposition were not addressed in the study, but the findings raise important questions in this regard that "may have profound therapeutic implications and deserve further investigation," they wrote.
By Eric Barnes
AuntMinnie.com staff writer
September 25, 2009
Related Reading
Contrast-enhanced perfusion echo bolsters treadmill stress tests, September 14, 2009
Dual-source CT angiograms can detect myocardial infarction. August 31, 2009
CARS report: Personalized medicine will dominate future care, June 26, 2009
PET/CT confirms presence of brown fat in adults, April 22, 2009
Myocardial steatosis in diabetics tied to reduced diastolic function, December 5, 2008
Copyright © 2009 AuntMinnie.com


















