A known anti-mammography screening research group has reignited the controversy over breast screening by claiming the technology’s benefits have significantly decreased over time while its harms (i.e., overdiagnosis) remain unchanged. Dr. László Tabár has issued a response.
The group of skeptics comprises Drs. Søren Christiansen and Henrik Støvring from the department of public health at Aarhus University in Denmark and Dr. Philippe Autier, an epidemiologist from the International Prevention Research Institute, Lyon.
In a paper published on 23 June in the European Journal of Public Health, they state that breast cancer mortality has decreased over the past three decades due to improvements in patient management and better therapies, while the number of women needed to be invited to mammography screening in Denmark to prevent one cancer death in 10 years has doubled.
"As the beneficial effects of mammography screening declines ever more, we should consider abandoning the current mammography screening program with biennial mammograms for everyone aged 50-70. Perhaps a more targeted, high-risk screening strategy could be an alternative, if studies showed the strategy's beneficial effects," Støvring, associate professor in the department of public health at Aarhus University, told AuntMinnieEurope.com.
"I think we are approaching a point where just continuing might become untenable from an ethical point of view, as fewer and fewer women will experience gains due to screening (they would not die from breast cancer anyway due to improved treatment), but the number of women harmed due to overdiagnosis and overtreatment remains constant," he noted.
Meanwhile, screening proponents reiterate that early diagnosis through breast screening is the key factor in mortality reduction and believe that the group's results are skewed.
Key findings
The study was based on 10,520 breast cancer deaths among Norwegian women between the ages of 50 and 75 between 1986 and 2016. The authors stated that the results were also applicable to the Danish population.
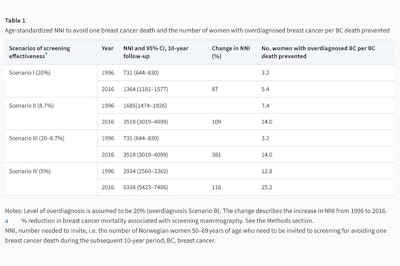
Improvements in therapy over the past 30 years have reduced mortality and this may erode the benefit-harm balance of mammography screening, according to the authors. They estimated that under the base case scenario of 20% breast cancer mortality reduction and 20% overdiagnosis, the number of women needed to be invited (NNI) to mammography screening to prevent one cancer death in 10 years rose from 731 (95% confidence interval [CI]: 644-830) women in 1996 to 1,364 (95% CI: 1181-1577) women in 2016, while the number of women with overdiagnosed cancer for each breast cancer death prevented rose from 3.2 in 1996 to 5.4 in 2016.
In another scenario, for a mortality reduction of 8.7%, the ratio of overdiagnosed breast cancers per breast cancer death prevented rose from 7.4 in 1996 to 14.0 in 2016. While, for a mortality reduction of 5%, the ratio rose from 12.8 in 1996 to 25.2 in 2016.
According to the authors, this shows that the benefit of mammography in terms of reduced mortality declines while the harms such as overdiagnosis are unaffected. Screening leads to both overdiagnosis and overtreatment, which has a cost both on a human level and in terms of the economy, they claim.
"One in five women aged 50-70, who is told they have breast cancer, has received a 'superfluous' diagnosis because of screening -- without screening, they would never have noticed or felt that they had breast cancer during their lifetime," noted Støvring.
In Denmark, women between the ages of 50 and 69 are invited to undergo a mammogram every second year. According to Støvring, a conservative estimate for the costs of the screening program would be at least 500 million Danish kroner (67.2 million euros) per year in a population of 5.8 million Danes.
"The first important observation is that 20% overdiagnosed is not among all women invited but among women diagnosed with breast cancer in the age group 50-70 years. In Denmark approximately 2250 per year are diagnosed in that age range," he continued. "450 per year are overdiagnosed, which is 20% of 2250."
Health professionals are a scarce resource, so it is vital to consider whether their time would be better spent treating other patients, since the benefits of mammography screening are becoming smaller, he said.
The authors further believe that future improvements to breast cancer patient management will increasingly reduce the benefit-harm ratio of screening.
As a recent participant in a colorectal screening program, Støvring has no issue with screening per se, but for breast cancer he believes that the evidence for mammography screening is not convincing.
"I think it is critical that we reassess screening programs as new evidence becomes available. There was once a screening for testicular cancer but the discovery of cisplatine-based therapies in the 1970s allowed the cure of most men diagnosed with it, even when metastases had spread to lymph nodes or distant organs. Because of this discovery, screening for testis cancer was progressively abandoned," he said.
Response from László Tabár
Breast imaging pioneer and early detection advocate Dr. László Tabár, professor emeritus of Uppsala University in Sweden, has disputed the authors' claims that the impact of early detection of breast cancer has declined.
Just the opposite happened, he noted, pointing to comprehensive studies from ongoing population-based service screenings that show a 50% decrease in breast cancer deaths, attributed to early detection and treatment in the early phase. He pointed out that to imply that the benefits of mammography screening were declining was an "unfortunate, deliberate fabrication."
 Dr. László Tabár
Dr. László Tabár"Our research group has done a contemporaneous comparison between the group that participated versus the group that did not participate in mammography service screening, which made it possible to evaluate the independent impact of early detection," he told AuntMinnieEurope.com.
"Dr. Støvring is not familiar with the 29-year follow-up results of the largest [randomized controlled trial], the Swedish Two-County trial, and also ignores the most recent publications of the ongoing nationwide, population-based mammography screening that evaluated the incidence of breast cancers fatal within 10 and 20 years after diagnosis among more than a half million Swedish women 40-69 years of age," he added.
Regarding the relative impact of early detection and treatment, Tabár noted that in countries with established mammography screening programs, cancer registries do not have information on the mode of detection (i.e., whether a cancer was detected among those who participated in screening versus those who did not participate) and therefore the relative impact of screening versus treatment in reducing breast cancer mortality cannot be evaluated based on registry data.
The authors' claims would appear to be plucked out of the air and have no scientific merit, he said. He also took issue with the title of the paper, pointing out that the randomized controlled trials never tested "screening" but "invitation to screening," and that this meant that mortality among those who were invited but never attended was also included in the results to make a correct comparison with the control group.
"I doubt that Dr. Støvring understands how to estimate overdiagnosis, but those researchers who calculated the rate of overdiagnosis after having adjusted for 1) lead time and for 2) the steadily increasing incidence of breast cancer, estimated the rate of overdiagnosis at 1-5%. Please compare the 50% decrease in breast cancer deaths among those who attend 'organized mammography screening' regularly with the shady statements about 'overdiagnosis'," Tabár said.
For further reading on this topic, Tabár urges members of AuntMinnieEurope.com to check out these three papers:
- Tabár L, Dean PB, Chen TH, Yen AM, Chen SL, Fann JC, Chiu SY, Ku MM, Wu WY, Hsu CY, Chen YC, Beckmann K, Smith RA, Duffy SW. The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer. 2019 Feb 15;125(4):515-523. doi: 10.1002/cncr.31840.
- Duffy SW, Tabár L, Yen AM, Dean PB, Smith RA, Jonsson H, Törnberg S, Chen SL, Chiu SY, Fann JC, Ku MM, Wu WY, Hsu CY, Chen YC, Svane G, Azavedo E, Grundström H, Sundén P, Leifland K, Frodis E, Ramos J, Epstein B, Åkerlund A, Sundbom A, Bordás P, Wallin H, Starck L, Björkgren A, Carlson S, Fredriksson I, Ahlgren J, Öhman D, Holmberg L, Chen TH. Mammography screening reduces rates of advanced and fatal breast cancers: Results in 549,091 women. Cancer. 2020 Jul 1;126(13):2971-2979. doi: 10.1002/cncr.32859.
- Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, Chiu SY, Chen SL, Fann JC, Rosell J, Fohlin H, Smith RA, Duffy SW. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011 Sep;260(3):658-63. doi: 10.1148/radiol.11110469



















