There are three vital requirements for thorough and effective cardiothoracic imaging, says Dr. Edwin van Beek, PhD, director of the Clinical Imaging Research Centre at Queen's Medical Research Institute at the University of Edinburgh in the U.K. The first is to fully reconstruct the field-of-view; volumetric CT with 1-mm reconstruction now provides a more complete picture of the chest than high-resolution 1-mm-slice CT did previously. The second is to promote collaboration between the cardiologist, pulmonologist, and the chest and heart radiologists. The third is that radiologists must ensure everybody can understand what the report means so that the referrer can be guided as to how to proceed.
"The patient's referrer is the shepherd, and the radiologist is the sheepdog. If the sheepdog spots a fox, it must bark," he told ECR Today in an interview ahead of the congress.
Persistence and attention to detail are important not just for the patient's well-being but also to avoid legal proceedings. He cites real cases of chest CT patients later experiencing an acute cardiac event. In these cases, coronary calcifications could be seen on CT but had, for one reason or another, been overlooked. Therefore, education in this area remains crucial.
Common reporting mistakes include not mentioning the coronary arteries in relation to age and gender, or calcifications of the aortic valve. van Beek, who is also Scottish Imaging Network (SINAPSE) chair of clinical radiology, points out that in a contrast CT scan, aortic valve stenosis and coronary artery disease can be visualized, as can anomalies in the pulmonary artery related to pulmonary hypertension.
"In the medicolegal area, our chief responsibility is for the clarity of the report," he said. "Cardiothoracic radiologists are working towards a lexicon but this is not the main solution. Instead, the answer is for our report to be thorough and understandable. We must bark loudly and clearly where required."
Evidence is increasing that chest CT can reveal alternative findings compared to clinical expectations. Regardless of the cardiopulmonary question, greater interdisciplinary collaboration, thorough reconstructions, and clear reporting styles are necessary to ensure pathologies in either the heart or lungs don't escape detection.
Delegates attending today's session will hear from experts how the cross-over in presentation between cardiac and pulmonary problems and their shared risk factors has led to growing demand for comprehensive cardiothoracic imaging for cardiopulmonary patients. Given the close interrelation of the lung and the heart, radiologists must always take a close look at the heart when assessing the lung and vice versa, say cardiothoracic imaging experts. This requires multiple reconstruction methods to visualize the whole chest cavity and dedicated focused areas of interest, plus an eye for alternative findings.
"In an aging population, it would be a mistake to only look at the lung aspects of a chest CT and ignore the cardiac aspects. The reverse is also true: cardiologists may ignore the noncardiac portion of a cardiac CT angiogram," said van Beek. "Lung cancer screening may show significant coronary calcifications, a direct predictor of a likely cardiovascular event over a five-year period. Similarly, lung cancer or emphysema may be revealed from cardiac studies; however, if you don't reconstruct the full field-of-view, these diseases will be easily missed."
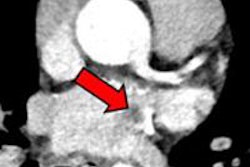
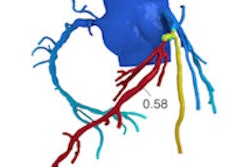
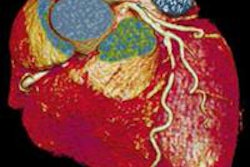
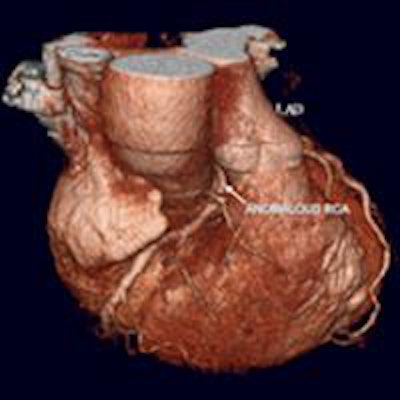
A case in point, van Beek remembers a CT scan that showed a right coronary artery anomaly (shown in figure below). He insisted on a reconstructed full field-of-view and discovered metastatic breast cancer, which changed management of the patient to extensive chemotherapy before coronary surgery. This also led to a shift in the cardiologist's mind at the time as to the usefulness of reconstructed full field-of-view images.
 Patient presenting with suspected anomalous right coronary artery. Coronary CT angiography shows interarterial right coronary artery (left, also shown on 3D reconstruction in center). Full field-of-view reconstruction reveals spiculated lung lesion, which proved to be metastatic breast cancer (right). Images courtesy of Dr. Edwin van Beek, PhD.
Patient presenting with suspected anomalous right coronary artery. Coronary CT angiography shows interarterial right coronary artery (left, also shown on 3D reconstruction in center). Full field-of-view reconstruction reveals spiculated lung lesion, which proved to be metastatic breast cancer (right). Images courtesy of Dr. Edwin van Beek, PhD.ECR 2016 delegates will also be reminded of the subtle information available on CT and MR such as abnormal shape (D-shaping) of the interventricular septum, which may indicate pulmonary pressure overload or how thickened interlobular septae and pulmonary ground-glass opacities on CT may point to pulmonary congestion secondary to heart failure.
In many patients with pulmonary diseases, the final lethal event is right heart failure. This occurs because the right ventricle, which supplies blood to the pulmonary artery, is not designed to cope with pressure overload associated with pulmonary hypertension.
 Left: Patient presenting with dyspnea. Contrast-enhanced CT chest demonstrates extensively calcified aortic valve with signs of heart failure. Right: Patient presenting with angina. The coronary CT angiography showed nonflow limiting coronary artery disease, but the full field-of-view reconstruction diagnosed lung cancer in the right middle lobe. Images courtesy of Dr. Edwin van Beek, PhD.
Left: Patient presenting with dyspnea. Contrast-enhanced CT chest demonstrates extensively calcified aortic valve with signs of heart failure. Right: Patient presenting with angina. The coronary CT angiography showed nonflow limiting coronary artery disease, but the full field-of-view reconstruction diagnosed lung cancer in the right middle lobe. Images courtesy of Dr. Edwin van Beek, PhD.Today the most relevant parameter for right ventricular function is measuring the ejection fraction by means of MRI. This parameter, which indicates how much percentage of its volume the heart can eject with each beat, is easy to measure and is an excellent parameter to predict outcome and to guide and monitor therapy, according to Dr. Jens Bremerich, head of the division of cardiothoracic imaging at the University Hospital of Basel in Switzerland. He will be presenting perspectives from cardiac imaging, specifically the role of the heart in cardiopulmonary disease.
At Basel University Hospital, there has been cooperation between cardiologists and radiologists for over 20 years, he explained. Prescriptions for cardiac imaging are seen by both cardiologists and radiologists, and approximately 1,000 cardiac MR studies per year, or around 20 per week, are read and then reported on by both parties. This relatively low volume of MRI versus 20,000 conventional chest x-rays and 5,000 chest CTs makes dual reading/reporting more feasible. These cases are also discussed locally between cardiology and radiology, with 10 cases covered in an hour-long session twice a week.
 Left: Patient with pulmonary hypertension. Conventional chest x-ray (A) shows enlarged pulmonary artery (white arrow); pulmonary circulation is compensated. Right: Contrast-enhanced CT yields enlarged right atrium (RA) and ventricle (RV). Hypertrophy of RV myocardium (arrowheads) indicate chronic RV pressure overload. Images courtesy of Dr. Jens Bremerich.
Left: Patient with pulmonary hypertension. Conventional chest x-ray (A) shows enlarged pulmonary artery (white arrow); pulmonary circulation is compensated. Right: Contrast-enhanced CT yields enlarged right atrium (RA) and ventricle (RV). Hypertrophy of RV myocardium (arrowheads) indicate chronic RV pressure overload. Images courtesy of Dr. Jens Bremerich."This setup is a little more costly than usual, but it is very interesting and provides an excellent setting for cardiology and radiology residents to train," Bremerich said. "I think all hospitals should strive to carry out dual reading and reporting in selected cases, and in general there should be a low threshold for exchange with the referrer in cardiothoracic imaging."
Originally published in ECR Today on 4 March 2016.
Copyright © 2016 European Society of Radiology