Noninvasive cardiac imaging techniques have developed considerably in recent years. The heart or coronary scan has profited from technological progress, improving the time taken to achieve resolution (under 100 ms) and widening the area of coverage (128-, 256-, or 320-detectors, dual-source technology), which allows acquisitions to be made by the latest generation machines in less than a heartbeat.
The gold standard is the 64-slice CT machine, especially in the emergency room (ER), and recent publications have stressed how useful the cardiac scan is for acute chest pain.
High negative predictive value of cardiac scans
The cardiac scan has a very high negative predictive value (more than 98%) throughout the series, including the versions offering 64 slices or more, and is able to rule out coronary origins if an examination proves normal. These data were underlined by the fact there were no major cardiac events occurring in patients with a normal heart scan, as confirmed by a recent study with a one-year clinical follow-up.1 Other studies, mainly conducted in the U.S., have shown the advantage of treatments incorporating a heart scan in the ER compared with traditional therapies involving hospitalization and noninvasive examinations, such as myocardial scintigraphy at a later date in patients at low or intermediate risk.2
The European recommendations issued in 2011 in relation to acute coronary syndromes had already classified the heart scan as a relevant examination (class IIa),3 but the new recommendations made in 2013 about stable angina confirm the growing place this technique has in treating patients, with the heart scan being recommended as the first intention treatment in symptomatic patients at low or intermediate risk (estimated risk between 15% and 20%).4 The new recommendations for 2013 included low-risk acute coronary syndromes (Figure 1).
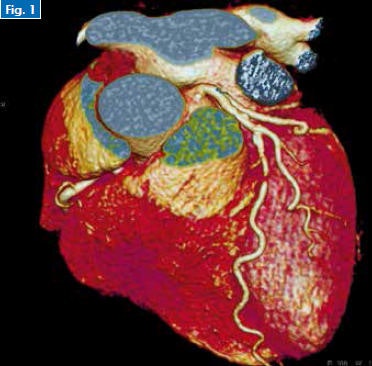 Figure 1. Cardiac CT scan for chest pain of an acute coronary syndrome type with a normal ECG and troponin levels shows tight stenosis of left anterior descending (LAD) II.
Figure 1. Cardiac CT scan for chest pain of an acute coronary syndrome type with a normal ECG and troponin levels shows tight stenosis of left anterior descending (LAD) II.What are the indications in the ER?
Employing this new treatment strategy can only be envisaged in close collaboration with cardiologists, as recommended in the charter signed by the French radiology and cardiology professional societies.5
Indications will be restricted to non-ST segment elevation acute coronary syndrome shown on the electrocardiogram (ECG) and with normal troponin levels (unstable angina), in patients at low risk of heart disease. It is impossible to perform these heart scans if there is any atypical chest pain in the ER, at the risk of being swamped with queries and having the whole technique discredited by indications that are wrongly diagnosed.
As far as this is concerned, the "triple rule out" -- consisting of simultaneously eliminating a pulmonary embolism, aortic dissection, and coronary stenosis -- is not strongly recommended in practice. It is more advisable to ask questions relating to a course of treatment defined by working together with emergency doctors and local cardiologists, in the awareness that a proximal pulmonary embolism may sometimes be "rectified" by a well interpreted heart scan.
Nevertheless, the contribution of the cardiothoracic scan in the differential diagnosis of acute chest pain (including acute aortic syndromes) must be emphasized.
The need for training
These new data may be validated very soon in France with proposals in line with the European recommendations. This makes it even more necessary for today's radiological community to undergo training in this technique of noninvasive cardiac imaging, especially because minimum knowledge of cardiac imaging is now essential for interpreting a chest scan (cardiothoracic) with high-speed latest generation scans. Apart from the aspect of synchronizing with the ECG and making rapid anatomical checks, it does not seem to be very complicated for a radiologist who regularly conducts angiograms of the carotids, kidneys, and lower limbs to quickly become able to recognize a normal, very diseased, or questionable heart scan (excluding coronary disease, coronary angiography, or continuing the assessment with ischemic imaging, respectively).
Manufacturers provide very acceptable training in the software used for heart problems and this software is increasingly rapid, intuitive, and ergonomic. Reports on the types of cardiac scans ought to be available online very soon on the sites of the professional societies, including the SFR (Société Française de Radiologie -- French Radiological Society) and SFICV (Société Française d'Imagerie Cardiaque Vasculaire -- French Society for Vascular Cardiac Imaging). It is easy to administer betablockers, and this must not prevent radiologists from becoming involved, especially as the general availability of the new high-speed machines in the future should limit their use.
What about MRI?
Cardiac MRI is very useful in the acute phase for revealing edema and/or myocardial necrosis, and it has been shown to be more sensitive than an ECG in diagnosing minor infarctions or sudden myocardial strokes. Nevertheless, cardiac MRI cannot be used at the moment in France in the emergency setting, even though it is used in other countries.
MRI is very useful in semiemergencies in acute coronary syndromes affecting "healthy coronaries," e.g., for diagnosing reperfused infarctions, myocarditis, or takotsubo syndrome. Moreover, the widespread use of the stress MRI is to be recommended in the early treatment of non-ST-elevation acute coronary syndromes at intermediate risk, especially as a partial replacement of myocardial scintigraphy or stress echocardiography.6 European recommendations on stable angina in 2013 validate stress MRI (perfusion) as a method equivalent to these two techniques, as confirmed by numerous studies.
The likely lack of technetium associated with the temporary closure of several reactors throughout the world (including the reactor in CEA Saclay Osiris) should strongly increase demand, and radiologists specializing in cardiovascular imaging ought to invest in this fast-developing method. Practical teaching workshops using simulation are available to show students how to handle the coronary vasodilating agents used and courses in the departments that regularly conduct this type of examination are accessible through the interuniversity diploma in cardiovascular imaging.
Only an investment by everyone, whether or not they are a specialist, will allow these new exciting techniques to remain within the radiological community.
Dr. Olivier Vignaux is a professor of radiology at Hôpitaux Universitaires Paris Centre, Université Paris Descartes, and a course leader in the whole-body MRI program organized by the CERF (Le Collège des enseignants de radiologie de France).
References
- Nasis A, Meredith IT, Sud PS et al. Long-term Outcome after CT Angiography in Patients with Possible Acute Coronary Syndrome. Radiology, 2014;272(3):674-682.
- Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. NEJM, 2012;366(15):1393-1403.
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). ESC Committee for Practice Guidelines. Eur Heart J, 2011;32(23):2999-3054.
- Montalescot G, Sechtem U, Achenbach S, et al. Task Force Members. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J, 2013;34(38):2949-3003.
- Joffre F, Boyer L, Dacher JN, Gilard M, Douek P, Gueret P. Recommendations for training in cross-sectional cardiac imaging. J Radiol 2009;90(9 Pt 2):1172-1175.
- Heitner JF, Klem I, Rasheed D, et al. Stress Cardiac MR Imaging Compared with Stress Echocardiography in the Early Evaluation of Patients Who Present to the Emergency Department with Intermediate-Risk Chest Pain. Radiology, 2014;271(1):56-64.
Editor's note: This is an edited translation of an article published in French on 20 October 2014 by the le Quotidien des JFR (Journées Françaises de Radiologie Diagnostique et Interventionnelle), the daily newspaper of the French national congress of radiology. Translation by Syntacta Translation & Interpreting.