In the setting of acute stroke, wavelet transform CT angiography (CTA) of the brain detects twice as many small-vessel occlusions as conventional single-phase CTA and provides substantially greater detail about them, researchers from Munich have found.
A study of 63 patients who appeared to have CT perfusion deficits, yet no evidence of vessel occlusion on conventional CTA and follow-up confirmation of acute stroke, showed that 31 vessel occlusions were visible in patients whose conventional CTA was negative, paving the way to vastly improved diagnosis and treatment.
 Dr. Wolfgang Kunz from the Institute of Clinical Radiology at Ludwig Maximilian University of Munich.
Dr. Wolfgang Kunz from the Institute of Clinical Radiology at Ludwig Maximilian University of Munich."Wavelet CT showed a significantly higher detail visualization of smaller vessels and vessel occlusions," Dr. Wolfgang Kunz said in a presentation at last month's ECR 2015.
Conventional or single-phase CTA in acute ischemic stroke allows reliable detection of large vessel occlusions in certain patients who are eligible for endovascular treatment, noted Kunz, who is from the Institute of Clinical Radiology at Ludwig Maximilian University of Munich. "As you might know from your daily routine, however, detection of small occlusions can be challenging."
Still, detection of small-vessel occlusions has been found to be a little easier in centers that use perfusion CT data to evaluate perfusion deficits -- that is, reconstructing their angiography imaging from CT perfusion data.
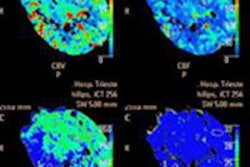
"Our institution developed wavelet-based reconstruction to improve contrast-to-noise ratio and visualization of collaterals," he said. "Our study aim was to assess the detection rate of vessel occlusions using this new wavelet based CTA in cases of patients who present with CT perfusion deficit -- this is measured as [cerebral blood volume] deficit -- and unremarkable CTA." However, follow-up MRI or CT within 72 hours confirmed acute ischemic stroke, he noted.
Wavelet transform algorithm applied to CT data
The researchers created images from whole-brain CT perfusion datasets after initial rigid-body motion correction using the wavelet transform (using the Paul wavelet, order 1) of each pixel attenuation time course. From these calculations, the angiographic signal intensity was extracted as the maximum of the wavelet power spectrum, they explained.
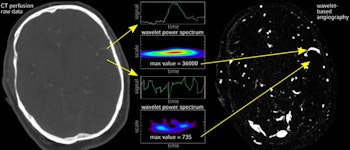
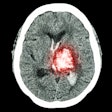
The wavelet transform of CT perfusion data is based on time-signal profiles (signal refers to HU values) of each voxel. Voxels with bolus flow time-signal profiles (upper arrows) are enhanced, whereas unspecific profiles (lower arrows) are suppressed. Note the higher detail visibility and contrast-to-noise ratio of small vessels. All images courtesy of Dr. Wolfgang Kunz.
"Wavelet transform is a very complex technical method [but] I will explain the basic idea," he said. First, the raw CT data yields a time-density (HU) profile over 45 seconds, "and if this resembles the bolus flow, which is happening in the arterial vessels, these structures will be enhanced in the final image," Kunz said. "On the other hand, if you have time-density profiles not resembling the bolus flow, like brain parenchyma or bony structures, these structures will be repressed and ... completely removed in the final image."
The cohort had 658 consecutive patients with suspected acute ischemic stroke who had undergone multiparametric evaluation including whole-brain perfusion CT due to suspected acute ischemic stroke.
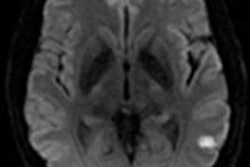
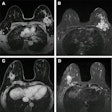
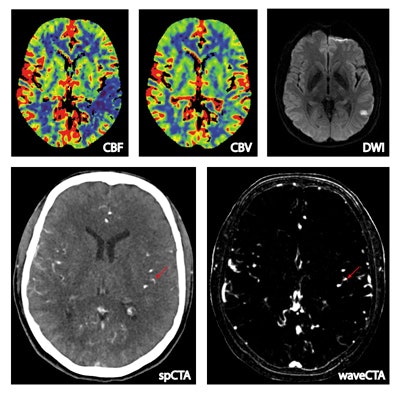 Above, a 55-year-old man presenting with right-sided hemiparesis and aphasia. Whole-brain CT perfusion (WB-CTP) shows a left-sided perfusion deficit in the middle cerebral artery territory with a mismatch between CBF und CBV. Follow-up MRI shows a relatively small final infarction volume. The wavelet-based CTA reconstructed from WB-CTP data demonstrates an M3 occlusion that is not evident in conventional CTA.
Above, a 55-year-old man presenting with right-sided hemiparesis and aphasia. Whole-brain CT perfusion (WB-CTP) shows a left-sided perfusion deficit in the middle cerebral artery territory with a mismatch between CBF und CBV. Follow-up MRI shows a relatively small final infarction volume. The wavelet-based CTA reconstructed from WB-CTP data demonstrates an M3 occlusion that is not evident in conventional CTA.Of these, 54.3% had a normal CT perfusion exam, and 45.7% (n = 287) had CT perfusion deficits. Among the 287 with perfusion deficits, 30% (n = 86) had a negative CTA exam, and among the 86 negative CTA patients, 73% had a confirmed stroke on follow-up CT or MRI within 72 hours. This left a final study population of 63 patients (mean age 74 years, range 34-89 years) with perfusion deficit, unremarkable CTA, but a confirmed stroke on follow-up.
Small vessel occlusions unseen at conventional CTA
Among the final study population of 63 patients, 31 had occlusions detected by wavelet CTA, most prominently in the middle cerebral artery (MCA), which yielded 48 cases, mostly on the M3 and M2 vessels, Kunz said. There were also smaller groups of anterior cerebral artery (ACA, n = 6) and posterior cerebral artery (PCA, n = 6) ischemias, among which wavelet CTP detected half, and finally three superior cerebellar artery occlusions, he said.
| Wavelet CTP-based detection of vessel occlusions among stroke patients with negative conventional CTA | |||
| Study population and stroke | Location | Vessel occlusions detected by wavelet CTA | Segment |
| Total | 63 | 31 (49.2%) | |
| MCA ischemia | 48 (76.2%) | 24 (50%) | M3 12 |
| M2 10 | |||
| M4 2 | |||
| ACA | 6 (9.5%) | 3 (50%) | A3 3 |
| PCA | 6 (9.5%) | 3 (50%) | P2 3 |
| SCA | 3 (3.7%) | 1 (33.3%) | |
The study team also rated image quality of the vessels between the two modalities. "We didn't see any differences in image quality in the larger vessels, but there was a significant difference in smaller vessels in the M2-M4 in favor of wavelet CTA," Kunz said.
Wavelet CT angiography shows significantly higher detailed visualization of small vessels and vessel occlusions in 49% of patients with CT perfusion deficit, negative CT angiography, and confirmed stroke at follow-up CT or MRI, he continued.
"We see possible applications in determining the impact of vessel occlusion on IV thrombolytic therapy outcomes," he said. "Notably our study population received IV therapy in about 50% of the cases." The technique could also be useful for differentiating strokes of unclear etiology, such as hemodynamic versus embolic strokes or second strokes.