The combination of ultrasound and MRI fusion-targeted biopsies with systematic biopsies is more effective for identifying suspicious lesions than systematic biopsies alone in cases of prostate cancer, Scottish investigators have found.
A team led by Cheng Wei, PhD, of the University of Dundee, U.K., also found that pre-biopsy, multiparametric MRI accurately identifies clinically significant prostate cancer.
"Ultrasound and MRI fusion-targeted biopsy combined with systematic random prostate biopsy had higher odds of depicting clinically significant lesions without incurring more procedure-related adverse events than either biopsy type alone," they concluded.
The best protocol for diagnosing clinically significant prostate cancer continues to develop, Wei and colleagues noted. Prostate cancer workup has traditionally been performed via systematic biopsy, but the technique can produce false-negative results and be vulnerable to undersampling, repeat biopsies, undergrading, and overdiagnosis or overtreatment of clinically insignificant disease.
Pre-biopsy, multiparametric MRI can identify clinically significant prostate cancer and reduces unnecessary biopsies and the overdiagnosis of clinically insignificant disease, the team explained; the current prostate cancer workup protocol consists of this type of MRI exam combined with MRI-guided targeted biopsies.
But could the two types of biopsies work well together? Wei's team sought to explore whether combining ultrasound and MRI fusion-targeted biopsies with systematic biopsies could offer greater diagnostic accuracy than either method alone.
The authors conducted a study that included 582 patients with suspected prostate cancer who underwent multiparametric MRI between January 2015 and August 2020. Of these, 413 had a PI-RADS score of at least 3 (intermediate -- and equivocal -- disease risk) and were randomized into either an intervention group that underwent ultrasound and MRI fusion-targeted biopsies with systematic random prostate biopsies (207, or 50.1%) or a control group which underwent systematic random biopsies alone (206, or 49.9%). The men underwent biopsy within a week after the multiparametric MRI exam.
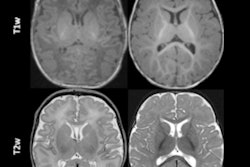
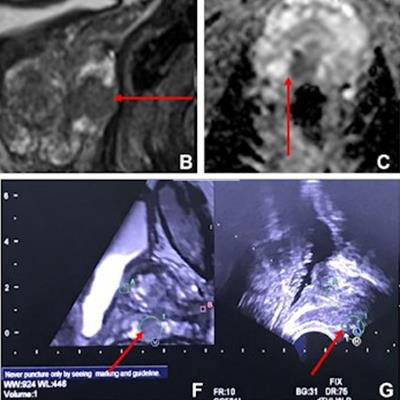
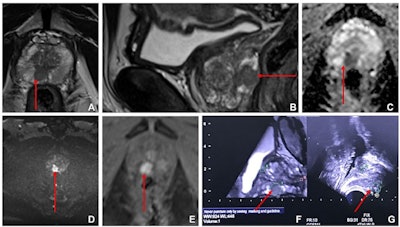 Images from multiparametric MRI of the prostate in a 60-year-old male participant show a focal lesion (arrow) in the right peripheral zone of the prostate at the mid-gland level. The lesion had low T2 signal on (A) axial and (B) sagittal T2-weighted MRI scans, marked corresponding restricted diffusion on (C) apparent diffusion coefficient and (D) high-b-value diffusion-weighted MRI scans, and (E) early contrast enhancement on a dynamic contrast-enhanced MRI scan. The lesion was a maximum of 13 mm on transverse axis with a bulge of the prostatic outline but no definite extraprostatic extension. This was scored as Prostate Imaging Reporting and Data System 4. Fused (F) isovolumetric T2 sequence with (G) US image. Square marker A is placed at the level of proximal prostatic urethra as an anatomic landmark. Fusion core showed a Gleason score of 3+4 prostate cancer. Images and caption courtesy of the RSNA.
Images from multiparametric MRI of the prostate in a 60-year-old male participant show a focal lesion (arrow) in the right peripheral zone of the prostate at the mid-gland level. The lesion had low T2 signal on (A) axial and (B) sagittal T2-weighted MRI scans, marked corresponding restricted diffusion on (C) apparent diffusion coefficient and (D) high-b-value diffusion-weighted MRI scans, and (E) early contrast enhancement on a dynamic contrast-enhanced MRI scan. The lesion was a maximum of 13 mm on transverse axis with a bulge of the prostatic outline but no definite extraprostatic extension. This was scored as Prostate Imaging Reporting and Data System 4. Fused (F) isovolumetric T2 sequence with (G) US image. Square marker A is placed at the level of proximal prostatic urethra as an anatomic landmark. Fusion core showed a Gleason score of 3+4 prostate cancer. Images and caption courtesy of the RSNA.Overall, the investigators found that the detection rate of clinically significant prostate cancer was higher in the intervention group, with an odds ratio of 1.79 (with 1 as reference). They also found that multiparametric MRI had a sensitivity of 72%, specificity of 71%, positive predictive value of 78%, and negative predictive value of 64% for correctly identifying clinically significant prostate cancer.
As for the biopsy arm of the study, among patients in the intervention group (fusion and systematic biopsy), 72.9% were found to have prostate cancer, versus 60.2% of men in the control group (systematic biopsy alone). In the intervention group, clinically significant prostate cancer was found in 62.8% of men, while in the control group, it was identified in 51.4% of patients.
In the control group, the adverse event rate after biopsy was 23%, and in the intervention group, it was 31%, but these percentages were comparable to rates for each type of biopsy alone, according to the researchers.
"[Our study showed that] pre-biopsy multiparametric MRI was accurate in the depiction of clinically significant prostate cancer ... [and that] combining ultrasound and MRI fusion-targeted biopsies with systematic biopsies helped detect more clinically significant lesions than did systematic biopsies alone," the group wrote.
The complete study can be found here.