Separate out the densest breasts from the less dense breasts in mammography screening programs: That's the message of German researchers. They found screening program performance decreases in these women when compared with the other, less dense categories.
In their large retrospective study that included more than 25,000 exams, the researchers analyzed the impact of breast density on breast cancer screening by dividing the number of screen-detected cancers by the sum of screen-detected plus interval cancers. The team, led jointly by Drs. Stefanie Weigel and Walter Heindel from the department of clinical radiology and reference center for mammography at the University of Muenster, found screening sensitivity was significantly lower in the densest breasts.
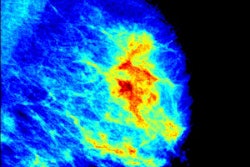
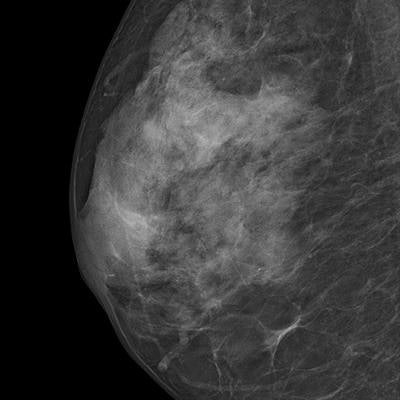
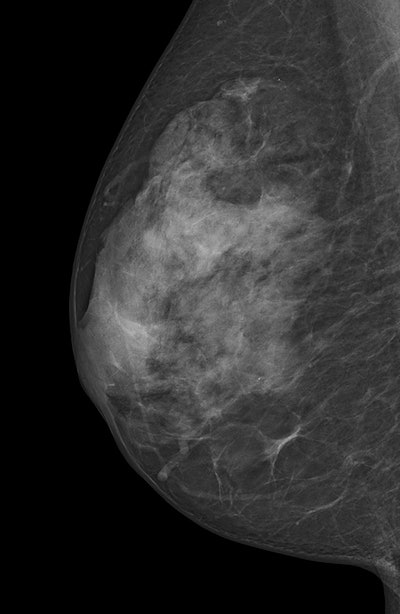 Digital mammogram of an ACR 3 dense breast. All images courtesy of Dr. Stefanie Weigel.
Digital mammogram of an ACR 3 dense breast. All images courtesy of Dr. Stefanie Weigel."We suppose that the screening performance should not be assessed in women with 'dense breast,' commonly derived from conflating women with ACR [American College of Radiology] 3 and ACR 4, but rather that it seems advisable to separate these two categories due to their different performance," they noted (European Radiology, 7 November 2016).
The problem with dense breasts
ACR's BI-RADS classifies breasts as almost entirely fatty (ACR 1), scattered areas of fibroglandular density (ACR 2), heterogeneously dense (ACR 3), or extremely dense (ACR 4). Heterogeneously dense and extremely dense are usually combined into one category of dense breasts. They are indicated by quartile ranges of percentage dense tissue more than 50% and as possibly obscuring small masses and lowering the sensitivity of mammography.
Most of the dense breasts are classified as heterogeneously dense and the frequency of breast densities is reported as 10% fatty, 40% scattered, 40% heterogeneously, and 10% extremely dense, the study authors explained. Higher breast density is associated with decreased mammographic sensitivity and specificity, as well as with increased breast cancer risk. Breast density may also be a factor that contributes differentially to screen-detected breast cancers and interval breast cancers, they added.
Weigel and Heindel analyzed the sensitivity of a population-based digital mammography screening program, taking specifically into account the impact of mammographic breast densities.
They studied women from a single digital screening unit of the National Mammography Screening Program in Germany, encompassing 25,576 double-read exams. They stratified the women ages 50 to 69 into each of the four ACR categories and found 192 screen-detected cancers and 48 interval cancers. The overall sensitivity of the program was 79.9%.
| Frequency and sensitivity per category | ||||
| 1st reading frequency | 2nd reading frequency | Sensitivity 1st reading | Sensitivity 2nd reading | |
| ACR 1 | 9.3% | 12.1% | 100% | 88% |
| ACR 2 | 43.4% | 43.9% | 83.9% | 85.7% |
| ACR 3 | 42.3% | 39.6% | 72.9% | 79.4% |
| ACR 4 | 5% | 4.3% | 50% | 50% |
Keep dense breasts separate
"The rate of breast cancers detected at screening was lower for breasts classified as ACR 4 than ACR 3 while the rate of interval cancers was higher, but these findings were not clearly significant," the authors wrote.
Worthy of note, however, is the average sensitivity of the program in women with ACR 3, as contrasted by sensitivity in ACR 4 of only 50% -- statistically significant irrespective of the reading-related classification selected.
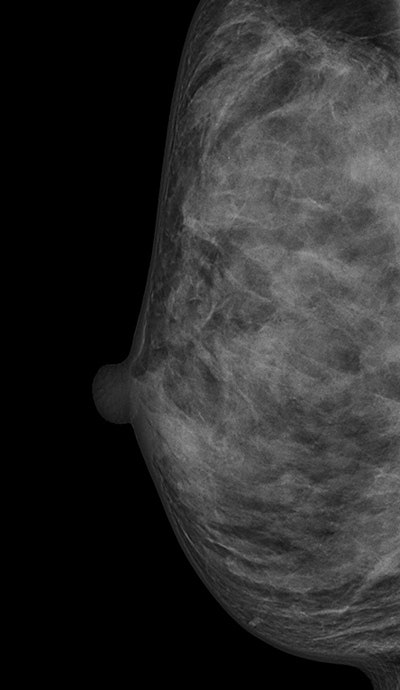 Digital mammogram of an ACR 4 dense breast.
Digital mammogram of an ACR 4 dense breast."In other words, only one out two breast cancer cases occurring among screening participants with ACR 4 over a period of 24 months was detected in the screening examination," they wrote. "Most likely, a varying extent of masking and obscuring of tumor signs -- if not associated with microcalcifications or architectural distortion -- in breasts consisting of up to 75% dense tissue (ACR 3) versus over 75% dense tissue (ACR 4) might lead to such a discrepant screening performance."
The lower sensitivity implies a shift of breast cancer diagnoses from the screening examination to the interval.
"In dense breasts, interval cancers were found to be phenotypically more similar to screen-detected breast cancers than interval cancers diagnosed in nondense breasts," the authors stated. "Therefore, interval cancers in dense breasts might be detected earlier with extended screening protocols. This may be especially useful with regard to the lobular subtype, as previous analyses in our digital mammography screening program revealed it was particularly low among young participants with lobular breast cancer."
The strengths of Weigel and Heindel's study are the prospective documentation of screening data gained in a clearly defined setting with validated protocols for all steps in the screening process.
A limitation is only one screening unit participated, and, thus, generalizability may be difficult. Also, automated software, which may increase the consistency of ACR classifications, was not available.
"Further research on criteria for objective standardization of ACR categorization and on the validation of these results in a multicenter setting is needed," the authors concluded.