Screening for breast cancer is not recommended for women younger than 40 who have normal, benign, or undocumented examination findings, but women with a moderate or high familial risk of breast cancer, personal breast cancer history, or those referred for screening are another story, Irish researchers have found.
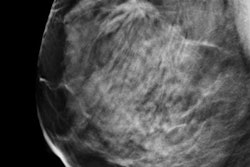
The researchers analyzed mammograms performed on patients 35 to 39 years old at St. James's Hospital in Dublin to determine the breast cancer detection rate for these younger women. The team, led by Dr. Anne Buckley from the department of diagnostic radiology, found only 2.1 cancer cases were detected per 1,000 women screened.
"This figure would be below accepted international thresholds to undertake screening mammography and raises radiation protection issues," the authors wrote (Clinical Radiology, 6 January 2017). "Additionally, a large number of benign biopsies were undertaken, with likely resultant psychological impact."
Why younger than 40?
In the U.K., best practice guidelines for patients presenting with breast symptoms state that mammography is not indicated for the majority of patients younger than 40 and breast pain alone is not an indication for imaging. In the Republic of Ireland, however, the National Quality Assurance Standards state that patients older than 35 presenting with breast symptoms should routinely have a two-view mammogram. There are no data, though, suggesting a benefit of this threshold.
Buckley and colleagues sought to determine the cancer detection rate based on the practice of referring women presenting to a symptomatic breast clinic who were between 35 and 39 with normal or benign clinical examination for bilateral screening mammography.
They excluded patients with moderate or high familial risk of breast cancer, personal breast cancer history or chest radiation, and general practitioner and internal hospital referrals and also males and those with abnormal clinical examinations. Included women had normal, benign, or undocumented examination findings.
After exclusions, the study consisted of 1,939 women. The researchers found four (0.21%) women were diagnosed with breast cancer confirmed at histology based on mammographic findings: two invasive ductal carcinoma (8 mm and 2 mm) and two ductal carcinoma in situ (DCIS; 4.5-mm high-grade DCIS and 2-mm low-grade DCIS). Overall, 115 biopsies were performed; 55 (47.8%) were attributable to mammographic screening, producing a biopsy rate of 2.8% due to mammography alone.
What does it mean?
Women between 35 and 39 years old form a large number of the patients attending breast clinics (approximately 12% of attendances at St James's Hospital in 2012), but they have a lower incidence of breast cancer than older groups, according to Buckley and colleagues.
"The present study had a biopsy rate of 5.93%, almost half of which would not have been performed if the women concerned had not undergone a mammogram," they added. "Although four cancers were detected among this subgroup, 51 invasive procedures were carried out on benign lesions. The additional biopsies driven by mammography in this cohort result in additional costs and also serve to increase patient anxiety."
The study authors noted that a limitation of their study was sample size -- larger numbers, greater than 6,000, would give a more definitive picture of the role of screening mammography in this demographic. However, as the data stand, screening women younger than 40 for breast cancer if they aren't at high risk has cost and resource implications for service providers, and it may have a psychological effect on the affected women.
The age threshold of 40 rather than 35 should be used to guide the age at which mammography is routinely used to evaluate women with breast symptoms, with the exception of women with higher risk in whom alternative thresholds are required, the authors concluded.