The prospect of growing legal costs in the Republic of Ireland's national breast screening program could threaten the ongoing viability of the service. The director of the program told news media on 24 May that she has received an increasing number of letters from lawyers representing women whose cancers may have been missed.
In an interview with RTÉ, the country's national radio service, BreastCheck National Clinical Director Dr. Ann O'Doherty said the program has received 15 letters from attorneys in the past two weeks for missed cancers, whereas usually the program deals with no more than one case a year.
O'Doherty said she was worried if the volume of legal inquiries continues, rising legal costs could threaten the viability of the BreastCheck program.
"Women who developed breast cancer between screenings over the last number of years are contacting solicitors," she said. "I'm not saying they've gone to litigation yet, and maybe they won't, but it is a huge concern, to see this amount of increased medical legal activity in a small amount of time."
O'Doherty told RTÉ the volume of legal inquiries ballooned in just the past two weeks, a trend she attributed to recent media coverage of breast screening. Mammography screening has been making headlines in the neighboring U.K. after revelations that a computer glitch in England's national screening program resulted in some 450,000 women not receiving their final invitation to screening.
While O'Doherty didn't specifically address the U.K. screening crisis, she noted the changing legal environment in the Republic of Ireland could necessitate the creation of some kind of mechanism for compensating women whose cancers were missed -- without bankrupting the program.
"I'm just worried about the medical-legal environment that has developed in the very recent weeks," she told RTÉ. "It's not that I don't think women who have been harmed should be compensated, I absolutely do, but we need some kind of forum where the legal profession, the medical profession, and other counseling services come together and afford women the opportunity to have a settlement that is commensurate with any damage, and doesn't divert huge taxpayer funds to legal costs and expert witnesses."
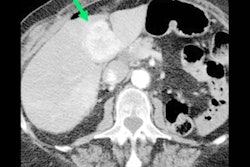
O'Doherty noted BreastCheck's goal is to reduce breast cancer mortality in the country by 20%. The service diagnoses some 2,600 women a year, with 680 dying from breast cancer. Interval cancers -- cancers that appear between rounds of screening -- occur at a rate of 9.6 cases per 10,000 women screened.
O'Doherty testified on 24 May before a national health committee on the growing legal issue, and said she's optimistic a solution can be worked out. Indeed, after her testimony, Irish politicians voiced their support for the program. Meanwhile, a solicitor who specializes in medical negligence said the 15 letters were not threatening legal action, but rather were from women asking for their medical records, according to an article on RTÉ's website.
Running the Irish Republic's breast and cervical cancer screening programs costs about 70 million euros a year, an amount that O'Doherty believes could be eaten up by litigation, especially if Ireland adopts an open disclosure law similar to the Statutory Duty of Candour law in the U.K., in which healthcare providers are required to notify patients if something goes wrong with their care.
"I'm hoping that we can sort this out and resolve it through mediation, getting doctors and lawyers to sit down together, and have a process that allows open disclosure without the cost to the taxpayer that will cost so much that we can't afford to screen," O'Doherty said.