In the future it will be essential to take into account the whole profile of the patient, including genetics, risk factors, and personal values and preferences, the research committee of the European Society of Radiology (ESR) has stated in a new white paper on personalized medicine.
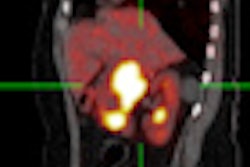
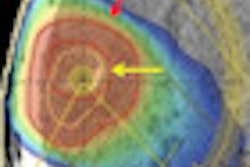
To adapt medical care to the individual situation, knowledge is needed, not only about the biochemical and physiological characteristics of the individual's disease, but also about location, extent, and inter- and intralesion heterogeneity. Biomarkers of different types must be combined to gain this knowledge, they argued. Genomics- and proteomics-based biomarkers are imperative, as are imaging-based biomarkers.
"For personalized medicine to reach its highest potential, medical imaging must be an integral part," the authors noted. "Each patient will expect completely individualized prediction, diagnosis, and treatment. Radiologists need to be prepared for this new paradigm as it will mean changes in training."
Personalized medicine should be included in postgraduate education and in research, and radiologists should have a stronger role in pharmacological research, they stressed in an online first article published on 30 September by Insights into Imaging.
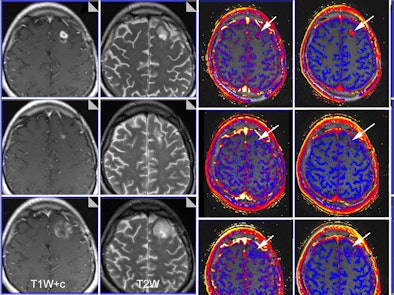 |
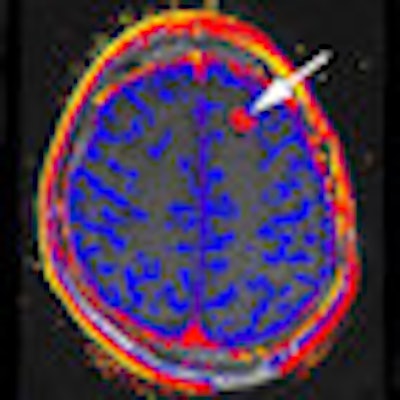
| Functional imaging biomarkers can provide important clinical information. In this case, multiparametric MRI was used to evaluate brain glioma response to bevacizumab therapy. Columns: T1-weighted images with contrast; T2-weighted images; transfer constant and leakage space. Rows (from the top): baseline, 10 days of therapy, and six weeks of therapy. Note that morphology imaging shows an initial response by the 10th day, but the tumor then progresses and is much larger at six weeks. However, functional images show that the drug is still working (reductions of transfer constant and leakage space - arrows). Images courtesy of Dr. Anwar Padhani, Paul Strickland Scanner Centre, Mount Vernon Cancer Centre, London. The images have been published in part in the following article: Padhani AR, Miles KA. Multiparametric imaging of tumor response to therapy. Radiology. 2010; Vol. 256:2, pp. 348-364. |
Overall, they think imaging plays a critical role in all aspects of personalized medicine: prediction, diagnosis, and especially treatment. Imaging is essential for excellent personalized medicine because it is the only patient-friendly means to obtain information on location, especially with regard to heterogeneous expression within an individual patient. Furthermore, imaging can also provide details about expression patterns, perfusion, metabolic activity, etc., which can be pivotal in deciding what the best treatment is and when is the best time to give it, the authors explained.
"The value of medical imaging in personalized medicine is frequently underestimated, as many policymakers forget the all-important right location in the paradigm," they wrote. "Medical imaging has always been personalized as it provides individual assessment of the location and extent of an abnormality. ... Stratification based on imaging biomarkers can help identify individuals suited for preventive intervention and can improve disease staging. In vivo visualization of locoregional physiological, biochemical, and biological processes using molecular imaging can detect diseases in presymptomatic phases or facilitate individualized drug delivery."
Personalized medicine is expected to have a major health-management impact in preventive medicine, in personalized diagnosis of disease, and in therapeutic decisions targeting specific alterations. Disease prevention depends on identifying -- in an early preclinical stage -- those subgroups of patients at risk of developing symptoms and signs of abnormal morphology and function. Identification of predictive biomarkers can help to monitor disease development and preventive interventions, they explained.
 Dr. Gabriel Krestin of Rotterdam chaired the ESR working group on personalized medicine.
Dr. Gabriel Krestin of Rotterdam chaired the ESR working group on personalized medicine.
The era of personalized medicine will mean changes for radiology, and the following are seen as areas of opportunity:
- Identification of predictive imaging biomarkers
- Visualization of cellular and molecular processes for early diagnosis of disease with the emerging discipline of molecular imaging
- Theranostics, or combining targeted imaging and targeted therapy, which enables the identification of heterogeneous and localized response to therapy
- Treatment monitoring, allowing early identification of treatment responders and nonresponders
- Identification of localized pathophysiology (perfusion, diffusion, metabolism) of diseased tissue
- Individualized, image-guided drug delivery systems
Implementing imaging-based personalized medicine strategies in clinical care is hampered by inadequate regulatory procedures, according to the authors. Both in Europe and in the U.S., new approaches to approval processes are needed, and the European Medicines Agency and Food and Drug Administration must acknowledge the crucial role of medical imaging in personalized medicine. However, they concede this is a complex proposition, given the mass of individual data and treatment options that arise.
The white paper was approved by the ESR Executive Council in June 2011. It was prepared by a working group chaired by Dr. Gabriel Krestin from Rotterdam, the Netherlands.