New radiological methods using other markers beyond the normal staging scan in endometrial cancer can help doctors stratify risk and manage patients better. That's the view of Prof. Andrea Rockall, clinical chair of radiology at Imperial College London.
Radiomics and body composition may have a key role to play in outcome prediction, noted Rockall, who is 2nd vice president of the European Society of Radiology ESR). She spoke on new imaging developments in endometrial cancer at the session about imaging and treatment of gynecological tumors during the ESR's connAction meeting on 2 June.
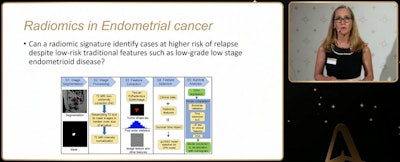 Typical workflow for radiomics where a patient's disease is identified on MRI with ensuing technical steps to identify survival time, as explained by Prof. Andrea Rockall at connAction.
Typical workflow for radiomics where a patient's disease is identified on MRI with ensuing technical steps to identify survival time, as explained by Prof. Andrea Rockall at connAction.Endometrial cancer is the most common gynecological cancer in Europe with increasing frequency due to growing incidence of obesity she told participants. Fortunately, most cases present at an early stage due to vaginal bleeding favoring good prognosis, she said.
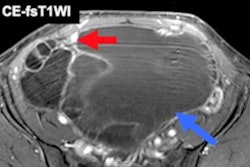
Both MRI and CT have been used for some time for staging to guide surgical planning. While MRI is used for local staging, gauging depth of endometrial invasion, cervical involvement, and local dissemination of disease in the pelvis, typically CT is used for staging the remainder of the chest, abdomen, and pelvis to look for the more advanced stages of disease. However, prediction of nodal metastasis remains challenging due to low sensitivity in normal-sized nodes, according to Rockall.
New research aims to provide more clarity on disease prediction. At Imperial, her group is working on radiomic analysis and body composition as biomarkers of outcome, and also studying how these new features can be incorporated in patient management.
Typically, patients will present with postmenopausal bleeding. Initial diagnosis usually takes place with ultrasound and biopsy. Usually, by the time patients undergo MRI or CT, the histological diagnosis is already made, noted Rockall.
"Treatment will typically include a simple hysterectomy and bilateral salpingo-oophorectomy (BSO) and on the radiological side, we let the surgeons know about cervical invasion, nodal enlargement and the more advanced stage, peritoneal disease," Rockall told participants. "But how can we potentially use radiomic signature and information about sarcopenia or fat distribution to give more information about likely outcome and how that might influence the way we manage the patient?"
Predictive models
Rockall pointed to the development of radiomic models that may help radiologists with certain predictions such as deep myometrial invasion, lymph node involvement, stage III or IV disease or provide survival analysis in nonendometrioid histology findings, by using the association of the signature with good or poor progression-free survival (PFS) and low or high hazard ratio.
At Imperial, Rockall's group has been looking at T2 sagittal MRI to determine whether radiomic signature can identify cases at higher risk of relapse despite low-risk traditional features such as low-grade, low-stage endometrioid disease.
"We're using an integrated approach which incorporates clinical features such as histology, patient age, as well as radiomic features combined to form a nomogram approach which can give one-year, three-year, and five-year predictions. This can improve prediction compared to using just the clinical features alone," she stated.
Sarcopenia and fat distribution is also an active area of research she told participants: Many women with endometrial cancer are obese and her group is trying to determine the impact on survival and whether it is modifiable.
"It may be that for patients with very aggressive tumors or advanced disease at presentation, sarcopenia and fat distribution - with the contribution of metabolic syndrome -- may not have an impact, but on long-surviving patients this could be of interest," Rockall said.
In one case, the use of an automated tool developed at Imperial College allowed sarcopenia measurements of the muscles at L3 to be collected from CT.
"We found that low risk endometrial cancer stratified by muscle density either below or above 34 Hounsfield units (HU) was a clear predictor for survival. In this case we haven't looked at very long survival ... but in longer term survival studies this may be of importance," she said.
Other areas of body composition such as liver fat may also be studied. Many patients with obesity will have fatty liver and some will develop NASH. She pointed to how there seemed to be some slight worsening of predicted outcome for patients with fatty liver, but without statistical significance. However, when looking at stage I endometrial cancer patients' PFS, those with a high level of visceral fat compared with subcutaneous fat had poorer outcomes.
Future steps
In the panel discussion with Imperial colleagues Dr. Stacey Bryan (gyne-oncological surgeon) and Dr. Laura Tookman (medical oncologist), Rockall noted that imaging-based staging with histology discussed with the multidisciplinary team may guide surgical extent.
The panelists underlined that it remained essential to work with surgical and oncology colleagues on guidelines and to identify the areas for potential improvement in care. These included the identification of high-risk patients for the correct planning of surgery and adjuvant therapy, the development of surveillance protocols, and the development of longer-term health support to reduce risks from obesity in women with endometrial cancer, where the cancer is low risk but there are high risks from other disease.
Thinking of future directions, Rockall's "research to do" list included work on radiomic signatures to improve patients' risk stratification, which might not only assist in nodal assessment for surgical planning but also in understanding surveillance mechanisms.
In addition, because body composition measurement can be easily automated, imaging that includes sarcopenia and fat distribution may allow improved identification of modifiable noncancer risk factors for survival, she noted. This would allow women the opportunity to take stock and potentially change lifestyle.
In terms of science, there is room for research on combining imaging with molecular markers that may further improve outcome predictions allowing doctors to understand where patients sit in the continuum of endometrial cancer from those that never need to be treated again to those that do, she noted.
You can watch the 60-minute session, "Gynaecological tumors: new developments in imaging and treatment - recommendations for clinical practice and directions for the future," on demand on the ESR website.