Award-winning research has underlined the value of advanced MRI techniques in illuminating the wide spectrum of clinical and imaging manifestations, differential diagnosis, and pitfalls in challenging cases of benign gynecological diseases.
"Common gynecological diseases may cause malignant transformation. Because early diagnosis may improve the patient's prognosis, clinical and imaging manifestations of malignant transformation should be well recognized," noted Dr. Mayumi Takeuchi, from the department of radiology, Tokushima University, Japan, and colleagues.
Recognizing the features of gynecological diseases with malignant transformation is vital to make a correct diagnosis and select the most appropriate therapeutic strategy, the researchers explained in an e-poster that received a magna cum laude award at ECR 2023.
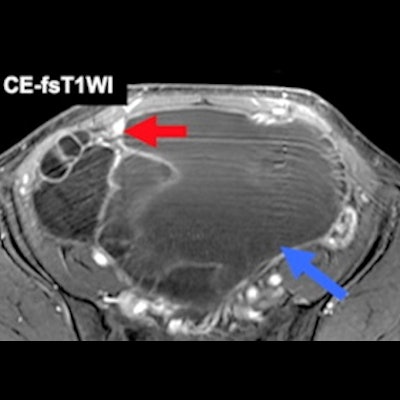
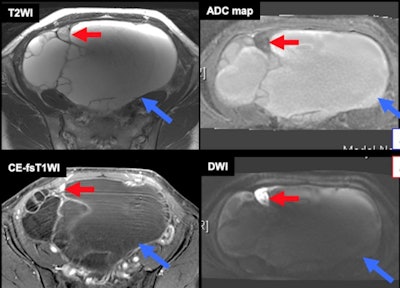 Metastasis within benign ovarian tumor. Some high-grade malignant tumors like serous tubal intraepithelial carcinoma (STIC) can metastasize to the ovaries or benign ovarian pathologies and mimic malignant transformation. Blue arrows = benign mucinous tumor. Red arrows = high-grade serous carcinoma. All images courtesy of Dr. Mayumi Takeuchi, Dr. Kenji Matsuzaki, and Prof. Masafumi Harada and presented at ECR 2023.
Metastasis within benign ovarian tumor. Some high-grade malignant tumors like serous tubal intraepithelial carcinoma (STIC) can metastasize to the ovaries or benign ovarian pathologies and mimic malignant transformation. Blue arrows = benign mucinous tumor. Red arrows = high-grade serous carcinoma. All images courtesy of Dr. Mayumi Takeuchi, Dr. Kenji Matsuzaki, and Prof. Masafumi Harada and presented at ECR 2023.Malignant transformation occurs in about 1% of cases of endometriosis (80% in endometriomas, 20% in extraovarian sites), and 90% are carcinomas and 10% are sarcomas, they pointed out.
The three types of malignant processes of endometriosis are epithelial cancers (endometrioid/clear cell carcinoma), other Müllerian-type tumors (seromucinous borderline tumor/mesonephric-like adenocarcinoma), and sarcomas (adenosarcoma, carcinosarcoma, endometrial stromal sarcoma). They generally affect women 10-20 years younger (5th-6th decades of life) than is the case in ovarian cancer without endometriosis.
"Because estrogen may have a role, patients of reproductive age should be treated, or followed closely," the authors noted. "Endometrioma is the precursor lesion for carcinomas via atypical endometriomas through pathways related to oxidative stress, inflammation, and hyperestrogenism and finally to genomic alterations."
Persistent oxidative stress induced by endometriosis-dependent hemorrhage may be associated with carcinogenesis, they added.
Main imaging findings
The definite imaging criteria includes the appearance of mural nodules; because T1-high hemorrhagic fluid may mask contrast enhancement of mural nodules, contrast-enhanced subtraction is useful. A malignant mural nodule shows high intensity on diffusion-weighted imaging (DWI) with a low apparent diffusion coefficient (ADC). Interval changes due to malignant transformation are dilution of hemorrhagic contents (disappearance of shading/T1-signal decrease) and interval enlargement of endometrioma.
"Clots in endometrioma may mimic malignant transformation," the authors wrote. "Contrast enhancement subtraction is critical for the differentiation. Susceptibility-weighted sequences may be also helpful in distinguishing clots from malignant transformation without administration of contrast medium, especially in patients with renal dysfunction, gadolinium allergy, asthma, or pregnancy."
Seromucinous borderline tumors consist of uncommon Müllerian-type tumors arising from endometriosis in at least a third of cases. They can affect younger women in their 30s and 40s, so fertility-preserving surgery may be considered.
Mesonephric-like adenocarcinoma are Müllerian-type tumors found in the uterine corpus and ovary. They may occur in endometriosis, and they affect mostly postmenopausal patients.
"Ovarian cancer may arise from adenomas/adenofibromas," the authors continued. "The solid variant of clear cell carcinoma (CCC) may arise from noncystic endometriosis via clear cell adenofibroma (CCAF) as CCAF-CCC sequence. CCAF components coexist in 15%-21% of CCCs and show lower tumor grade and better prognosis. T2-low fibrous areas within solid components are frequently observed."
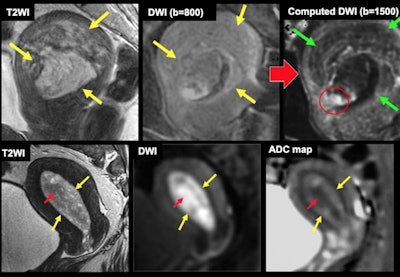 Endometrial cancer in endometrial polyp (top row of three images): the cancerous focus is clarified due to signal decrease of polyp on high b values on computed diffusion-weighted imaging (DWI). Endometrial cancer in endometrial hyperplasia (bottom row of three images): the cancerous focus is well visualized as low apparent diffusion coefficient (ADC) area on ADC map. Red arrows = cancer. Yellow arrows = polyp/hyperplasia. Green arrows = signal decrease of polyp on high b values on computed DWI.
Endometrial cancer in endometrial polyp (top row of three images): the cancerous focus is clarified due to signal decrease of polyp on high b values on computed diffusion-weighted imaging (DWI). Endometrial cancer in endometrial hyperplasia (bottom row of three images): the cancerous focus is well visualized as low apparent diffusion coefficient (ADC) area on ADC map. Red arrows = cancer. Yellow arrows = polyp/hyperplasia. Green arrows = signal decrease of polyp on high b values on computed DWI.It is also important to be aware of endometrial polyp/hyperplasia with malignant transformation, they noted.
Type I endometrial carcinomas are low-grade tumors that affect younger women, and they are associated with hyperestrogenism and arise from hyperplasia. Type II carcinomas are high-grade tumors affecting postmenopausal women, and they have aggressive behavior and arise from atrophic endometrium or polyp.
Endometrial hyperplasia/polyp may show high signal intensity on DWI, but they show high ADC ("T2 shine-through") and signal decrease on high b-value in computed DWI, whereas cancer shows low ADC but high signal on high b-value in computed DWI.
To view the whole ECR 2023 poster and learn more about the full range of findings and procedure details, go to the EPOS section of the congress organizers' website.
The co-authors of the ECR e-poster were Dr. Kenji Matsuzaki, from Tokushima Bunri University, Sanuki, Kagawa, and Prof. Masafumi Harada, from Tokushima University.