A new multidisciplinary study has suggested that pancreatic cancer remains a notoriously difficult diagnosis. In 600 confirmed cases of pancreatic cancer, 46 patients failed to have their cancer diagnosed through their first scan, representing a missed cancer rate of 7.7%.
Dr. Nosheen Umar, a gastroenterology research fellow at the University of Birmingham, U.K., and colleagues analyzed postimaging pancreatic cancer (PIPC) case records for the 2016-2021 period. The patients had a median age of 76 years, and 59% were women. Half came from the Sandwell and West Birmingham NHS Trust and half from the Leeds Teaching Hospitals NHS Trust, and they all subsequently received a pancreatic cancer diagnosis between three and 18 months after the initial investigation.
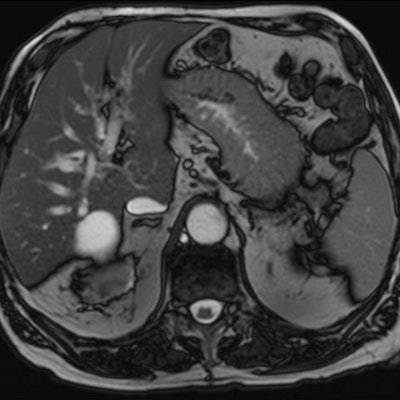
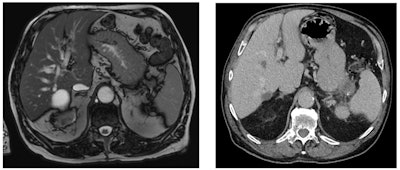 On two scans taken six months apart, a pancreatic tumor (stage IVB) was missed. On the MRI for renal cancer restaging six months prior, the lesion in the tip of the pancreatic tail was small and visible in retrospect only. Figure courtesy of Dr. Nosheen Umar.
On two scans taken six months apart, a pancreatic tumor (stage IVB) was missed. On the MRI for renal cancer restaging six months prior, the lesion in the tip of the pancreatic tail was small and visible in retrospect only. Figure courtesy of Dr. Nosheen Umar.Umar presented the group's preliminary findings at the United European Gastroenterology (UEG) Week, which is being held in Vienna from 8 to 11 October. The analysis revealed over one-third (36%) of the PIPC cases were potentially avoidable, she said.
Abdominal and pelvic CT and MRI scans were independently reviewed by radiologists to develop an algorithm to categorize the missed cases and identify the most likely explanation for why they were missed.
The researchers found that in 10% of PIPC patients, imaging signs associated with pancreatic cancer, such as dilated bile or pancreatic ducts, were not recognized as such and not investigated further.
In the previous scans of 13 patients (26%), the signs of a mass lesion were not picked up by the radiologist, Umar added.
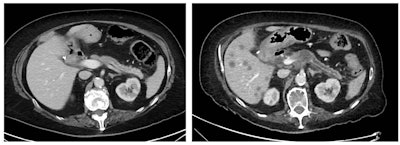 On two scans taken six months apart, a pancreatic tumor (stage IIIA) was missed, with the lesion being visible on review. Low attenuation area proximal body and minimal pancreatic duct dilatation distally were not reported. Figure courtesy of Dr. Nosheen Umar.
On two scans taken six months apart, a pancreatic tumor (stage IIIA) was missed, with the lesion being visible on review. Low attenuation area proximal body and minimal pancreatic duct dilatation distally were not reported. Figure courtesy of Dr. Nosheen Umar.There is often only a very short period for curative surgery in pancreatic cancer, meaning it is vital that patients are diagnosed with the disease as early as possible, she said. Also, it would be "interesting to know how many outcomes would be different with earlier age detection," noted Umar.
Feedback from radiologists
The rate of 7.7% missed tumors was "not a surprise," and other researchers have reported similar findings, Prof. Luis Marti-Bonmati, chairman of the radiology department and director of medical imaging at La Fe University and Polytechnic Hospital in Valencia, Spain, told AuntMinnieEurope.com.
"The identification rate of pancreatic cancers are dictated by the size of the lesion and the amount of isoattenuating small tumors," explained Marti-Bonmati, who was made a gold medallist of the European Society of Gastrointestinal and Abdominal Radiology in 2018. "The imaging technique is critical to the success in identification of pancreatic cancers."
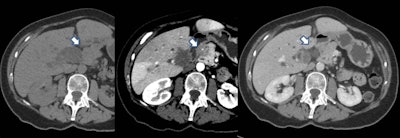 The tumor is not visible on either the precontrast scan or in the portal venous phase. It is only visible as a hypovascular mass on the later arterial phase. This technique is important when looking for pancreatic cancer. Courtesy of Dr. Alexandre Pérez Girbes, La Fe University and Polytechnic Hospital, Valencia, Spain.
The tumor is not visible on either the precontrast scan or in the portal venous phase. It is only visible as a hypovascular mass on the later arterial phase. This technique is important when looking for pancreatic cancer. Courtesy of Dr. Alexandre Pérez Girbes, La Fe University and Polytechnic Hospital, Valencia, Spain.In CT, the dose concentration and rate of contrast administration are vitally important to identify pancreatic tumors, and the use of spectral CT or dual-energy CT scanners can help to pick up isoattenuating tumors at low or standard energy, he pointed out. For further reading in this area, Marti-Bonmati recommends the recent "Insights into Imaging" article by Dr. Hongwei Liang and colleagues.
There is always a certain rate of missed cancers, sometimes because of underlying confounding factors, such as chronic pancreatitis mimicking or masking a mass, noted Dr. Rossano Girometti, associate professor of radiology at Udine University Hospital in Italy. "It can be a difficult diagnosis, even for the pathologist," he said.
He added that a pancreatic lesion may be missed because the case is inherently difficult, such as isodense cancers or cancers arising in a chronic pancreatitis context, and this can happen because of the nature of the lesion or pancreatic background.
Serious professional issues may be involved too, according to Girometti. "While the study represents a nice audit, it also emphasizes that some cancers are not difficult to detect per se, but are rather missed, thus prompting the need for strategies to overcome this bad outcome, e.g., involving experienced radiologists, less tired radiologists, and so on."
Overall, symptoms can be hard to identify, and many patients are diagnosed at a late stage because the disease often only presents vague early symptoms, such as jaundice, abdominal and back pain, unexplained weight loss, and nausea, Umar stated. The complex nature of the disease also makes screening for early diagnosis challenging to implement.
Pancreatic cancer is the third-leading cause of cancer-related deaths in the European Union after lung and colorectal cancers, accounting for around 95,000 deaths a year. More than 80% of patients who develop pancreatic cancer have locally advanced or metastatic disease at diagnosis and median overall survival times of less than 12 months. Life expectancy at the time of diagnosis is only 4.6 months.
Need for standardization
 Dr. Nosheen Umar, University of Birmingham.
Dr. Nosheen Umar, University of Birmingham.Umar emphasized that this was only a preliminary study from two sites in the U.K. and that further research needs to be conducted nationally. She hopes the study will raise awareness of the issue of postimaging pancreatic cancer and common reasons why pancreatic cancer can be initially missed.
"This will help to standardize future studies of this issue and guide quality improvements efforts, so we can increase the likelihood of an early diagnosis of pancreatic cancer, increase the chances of patient survival, and, ultimately, save lives," she said.
The senior author of the study was Dr. Nigel Trudgill, a consultant gastroenterologist at Sandwell and West Birmingham NHS Trust and the chair of the esophageal committee of the British Society of Gastroenterology. The coauthors were Dr. Justin Smyth, hepatobiliary radiology registrar at University Hospital Birmingham; Dr. Melisa Sia, hepatobiliary radiology registrar at Leeds Teaching Hospital; Dr. Raneem Albazaz, consultant radiologist at Leeds Teaching Hospital; Dr Umair Kamran, gastroenterology registrar at Sandwell and West Birmingham NHS Trust; and Dr. Mohan Brinder, consultant radiologist at University Hospital Birmingham.



















