Microultrasound has detection rates for prostate cancer that are comparable to multiparametric MRI in men who have not yet been biopsied, a Canadian study published on 19 July in Radiology found.
Researchers led by Dr. Sangeet Ghai from the University of Toronto also found that while microultrasound is inferior to MRI for avoiding biopsy, most lesions visible on MRI are also visible on microultrasound.
"Where access to MRI is limited or has contraindication to MRI, say hip prosthesis or a pacemaker, [microultrasound] can detect lesions which would have likely not been seen on conventional ultrasound," Ghai told AuntMinnie.com. "Even when used with MRI, the MRI lesions are most of the time visible on microultrasound and therefore one does not need fusion for accurate targeting."
Multiparametric MRI is superior to transrectal ultrasound when it comes to detecting lesions in the prostate. By combining images from T2-weighted, diffusion-weighted, and dynamic contrast-enhanced protocols, and sometimes MR spectroscopy, the multiparametric method produces more detailed 3D images of the prostate gland than through conventional MRI.
However, the researchers wrote that this method faces the challenges of higher cost, access, and interpretation challenges, and it also requires expertise in image-guided biopsy with fused images. Along with that, they added that multiparametric MRI has "moderate" interobserver agreement between readers and variability in scan quality.
Microultrasound operates at frequencies up to 29 MHz, and researchers have been looking into its potential for prostate cancer diagnosis. Microultrasound transducers have a fourfold higher crystal density, which makes for improvement of spatial resolution to as low as 70 mm, the size of a prostate duct. The investigators have also touted this method's higher sensitivity compared with transrectal ultrasound. However, microultrasound is also susceptible to interobserver variability in interpreting images.
In the current study, Ghai and colleagues wanted to compare microultrasound and multiparametric MRI and microultrasound in detecting clinically significant prostate cancer (grade group ≥ 2) and find out the proportion of MRI nodules visible at microultrasound for real-time targeted biopsy. They looked at data from 94 men with an average age of 61 years.
The authors found that microultrasound and MRI-targeted biopsy detected prostate cancer in 33 and 37 of the men, respectively (p = 0.22). They also found comparable results for clinically insignificant prostate cancer (p = 0.99), as well as cribriform and/or intraductal prostate cancer (p = 0.99).
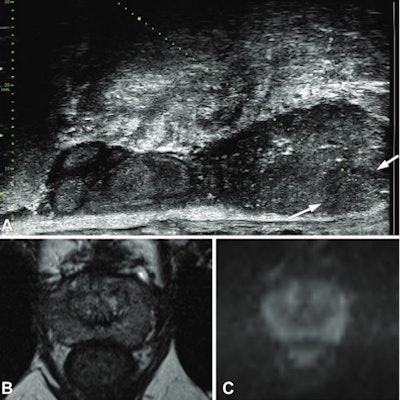
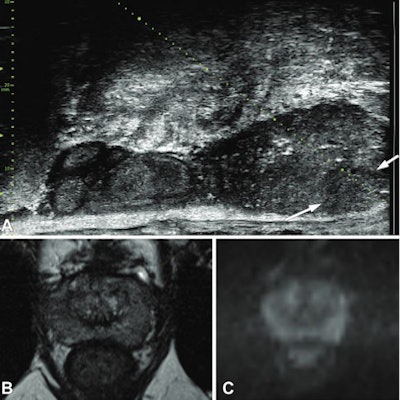 Images show a 49-year-old man with prostate-specific antigen (PSA) level of 8.26 ng/mL. (A) Prostate risk identification was performed with microultrasound on a category 4 nodule (arrows) in the left midgland peripheral zone. The lesion was not identified at multiparametric MRI. Corresponding T2-weighted (B) and high-b-value diffusion-weighted (C) MRI scans are also shown. Targeted biopsy revealed grade group 2 disease. Images courtesy of the RSNA.
Images show a 49-year-old man with prostate-specific antigen (PSA) level of 8.26 ng/mL. (A) Prostate risk identification was performed with microultrasound on a category 4 nodule (arrows) in the left midgland peripheral zone. The lesion was not identified at multiparametric MRI. Corresponding T2-weighted (B) and high-b-value diffusion-weighted (C) MRI scans are also shown. Targeted biopsy revealed grade group 2 disease. Images courtesy of the RSNA.The MRI- plus microultrasound-targeted biopsy pathway showed clinically significant prostate cancer in 38 men (40%). The researchers also found that nontargeted systematic biopsy compared to MRI- plus microultrasound-targeted biopsy did not allow clinically significant prostate cancer to be identified in any additional men. However, it helped identify nine additional men with clinically insignificant prostate cancer (p = 0.04).
Additionally, microultrasound kept just nine of the 94 men from avoiding biopsy while MRI helped avoid biopsy in 32 men from the total cohort (p = 0.001).
Among 93 MRI targets, researchers found that 62 (67%) were prospectively visible on microultrasound.
The study authors wrote that their results show that microultrasound is an attractive addition to multiparametric MRI in detecting clinically significant prostate cancer, with both modalities complementing each other.
"The fact that microultrasound also detected cribriform and intraductal cancer was a bonus and has not been published previously," Ghai told AuntMinnie.com. "Additionally, we feel that microultrasound will be a very good fit with bi-parametric MRI in the future."
The team added that multicenter randomized trials comparing the two techniques are needed to validate their findings and establish microultrasound for diagnostic settings.